Author:
Kai Knudsen
Updated:
8 January, 2026
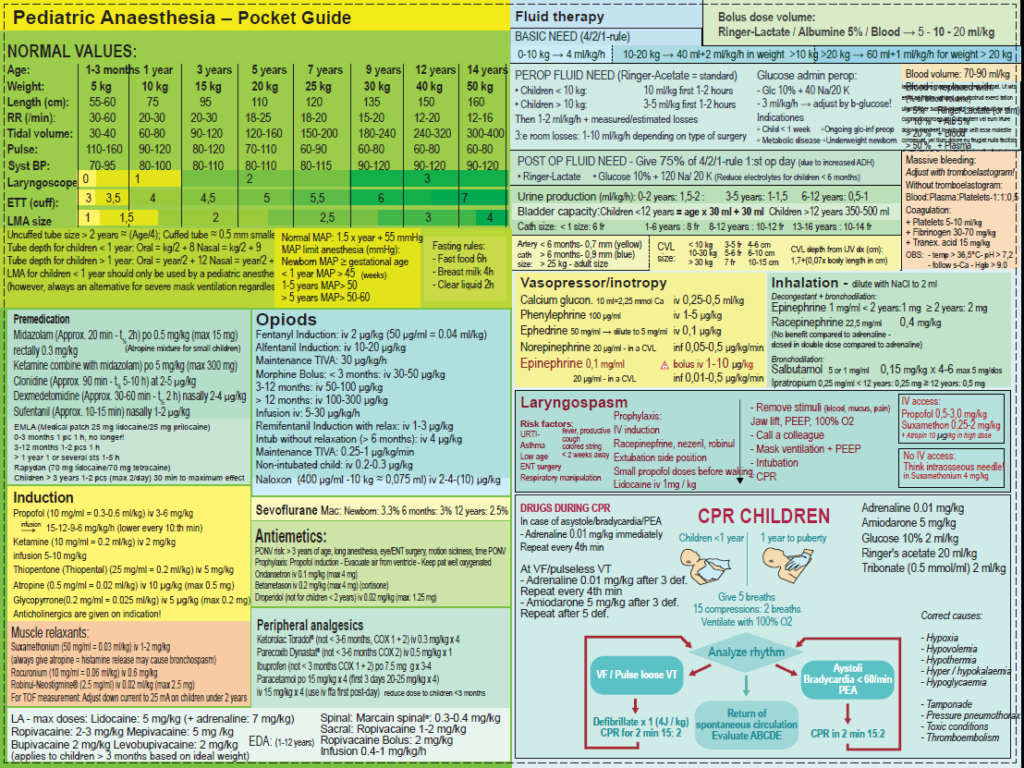
In this chapter, the various aspects of pediatric anesthesia are thoroughly described. Here, you will find normal physiological values as well as the correct tube sizes, appropriate medications, and correct dosages for children of different ages and weights. Practical steps for performing pediatric anesthesia with modern techniques and good safety are described here.
- Premedication for children. Sedation of children.
- Clonidine
- Dexmedetomidine
- Paracetamol
- Benzodiazepines
- Ketamine
- Practical advice before anesthesia for children
- Maximum doses of local anesthetics for children
- Size of endotracheal tubes for children
- CVC sizes for children
- Laryngeal mask for children
- Laryngoscope / Blade Size for children
- Pediatric Anesthesia Pocket Guide
- TIVA for pediatric anesthesia
- Circulation hemodynamics
- MAC values for children during inhalation anesthesia
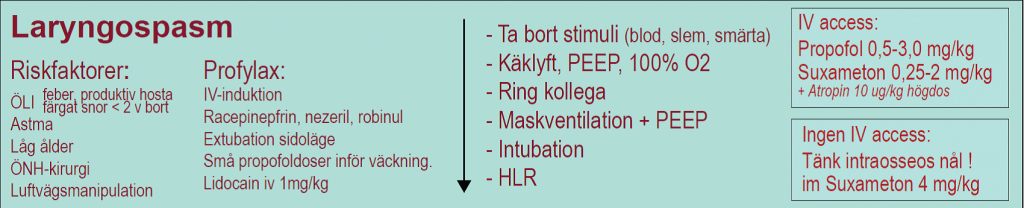
- Laryngospasm in children
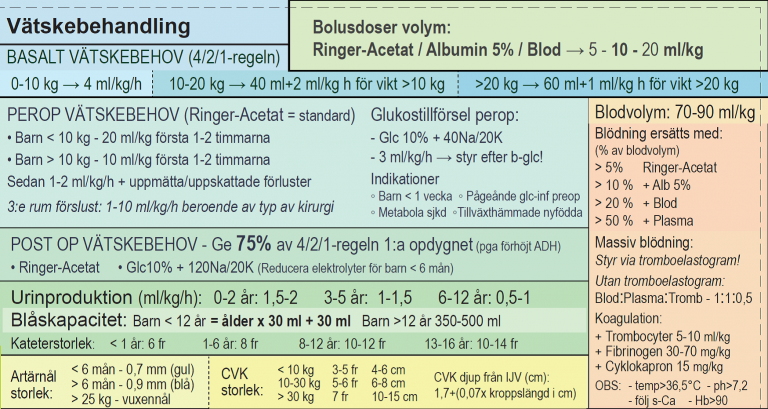
- Fluid therapy for children
- Bleeding
- Mechanical Ventilation of Children
- Difficult Airway Management
- Sedation of Children on a Ventilator
- Optiflow (High-Flow Nasal Cannula) for Children
- Resuscitation of Children
- CPR for Children
- A-CPR for Children
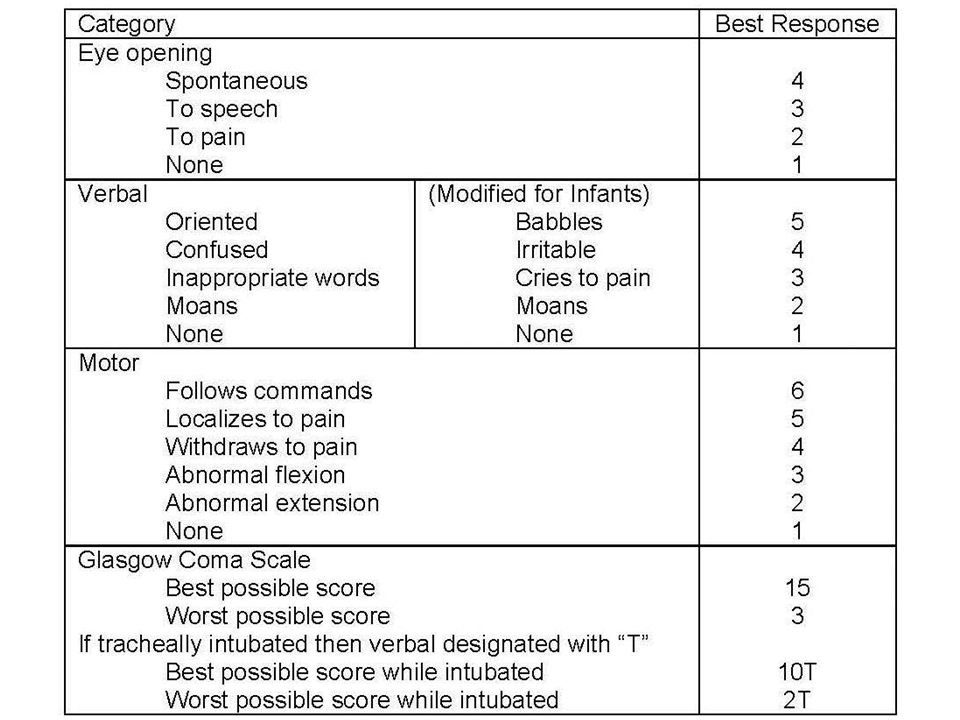
- Glasgow Coma Scale for Children
- Topical Anesthesia for Skin
- Vascular Access
- Central Lines
- Arterial Needles
- Nutrition for Children
- Enteral Nutrition
- Parenteral Nutrition
- Pain Assessment Scale for Children 0-7 Years
- Syringe Sizes for Medications for Children
- Thromboprophylaxis in Immobilization
- Urine Production in Children
- Antiemetics for Children
- Premedication with Intranasal Sufentanil for Children
- Acute Poisoning in Children
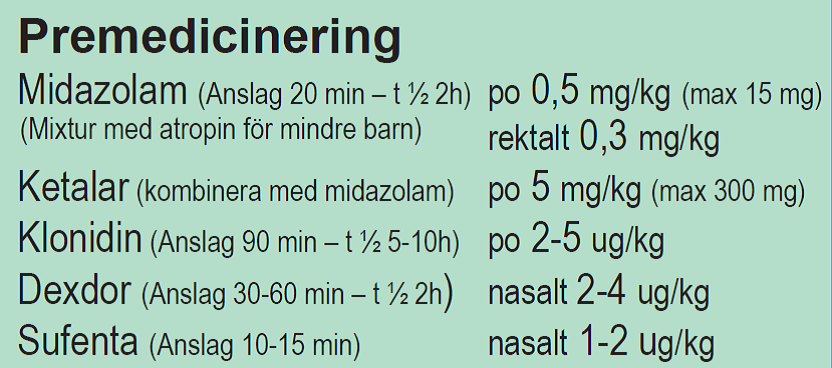
Premedication for children. Sedation of children.
There are a variety of medications used in premedication for children to achieve analgesia and anxiolysis. The main principle is that these medications should be pain-relieving and relaxing. The general preoperative care of children with parents is essential to gain the trust of the patient and parents for a good and safe anesthesia induction. Frightened and anxious parents can easily transfer their anxiety to the child, so preoperative information is crucial. During anesthesia induction, it is advisable for only the calmest parent to be present.

Sedation
- Mild sedation = “anxiolysis”
- Moderate sedation = “conscious sedation”
——> Borderline for maintaining airway reflexes and unaffected breathing = Borderline for fasting and IV access! <——
- Deep sedation
- General anesthesia
Premedication
- Paracetamol orally 30 mg/kg
- Midazolam (Onset 20 min – t ½ 2 h) po 0.5 mg/kg (max 15 mg)
- Midazolam rectally 0.3 mg/kg
- Ketamine (Ketalar) (combine with midazolam) po 5 mg/kg (max 300 mg)
- Clonidine (Catapresan) Time to onset 90 min – t ½ 5-10 h) po 2-4-6 μg/kg
- Dexmedetomidine (Dexdor). Onset 30-60 min – t ½ 2 h) nasally 2-4 μg/kg
- Sufenta (Sufentanil). Onset 10-15 min – nasally 1-2 μg/kg
Clonidine
Dosage: 2-5 μg/kg orally, provides good sedation in premedication. The downside is that the drug has a long onset time and must be given well in advance, 60-90 minutes before. Premedication with Clonidine hydrochloride Mixture 20 μg/ml or Clonidine Tablets 75 μg.
Dosage
Dosage range: 2-4-(6) μg/kg. Dose: We recommend 3 μg/kg. Children < 3 years and all ENT children 2-3 μg/kg. Ex; child weight 15 kg x 3 μg/kg = 45 μg and 2.2 ml (20 μg/ml) clonidine hydrochloride.
Dexmedetomidine and Clonidine for children
| Dexmedetomidine 100 µg/ml | Clonidine 150 µg/ml | |||
|---|---|---|---|---|
| Intravenously | Intranasally | Intravenously | Orally | Epidurally (Epi) |
| 1 µg/kg (max. 200 µg) by infusion or slow injection | 1,5-2 µg/kg (MR 4 µg/kg) Max 200 µg | 1-4 µg/kg x 3 | 1-4 µg/kg x 3 | 0,1-0,3 µg/kg/tim |
Dexmedetomidine
Provides good premedication for young children coming for ear, nose, and throat procedures. Dexmedetomidine (Dexdor®) 100 µg/ml injection can be administered nasally or buccally. Nasal administration is preferred as it provides better absorption and faster effect. The solution has no taste and does not sting in the nose. Dexmedetomidine is a specific alpha2 receptor agonist and its effect is similar to Clonidine, but with more pronounced effects. The main effects are sedation and some analgesia. Dexmedetomidine has a shorter half-life, about 2 hours compared to Clonidine’s 5-10 hours. The onset time is significantly longer compared to orally administered Midazolam, approximately 20-40 minutes.

Dosage
Children 1-3 years old receive 1 µg/kg. Children 3-10 years old receive 1-2 µg/kg. Children over 10 years old receive 1-3 µg/kg. The dose can be increased with age up to a maximum of 3 µg/kg. Nasal administration is simplest with MAD (Mucosal Atomization Device) or MADdy (pediatric variant) connected to a syringe. The prescribed dose of medication is diluted to the desired volume (usually 0.3-0.5 ml) with physiological saline solution.
Reasonable dose for dexmedetomidine nasal 100 microg/ml
| 1 kg | 5 kg | 10 kg | 50 kg | |
|---|---|---|---|---|
| 1 mikrog/kg | - | - | 0,1 mL | 0,5 mL |
| 2 mikrog/kg | - | 0,1 mL | 0,2 mL | 1 mL |
| 3 mikrog/kg | - | 0,15 mL | 0,3 mL | 1,5 mL |
Monitoring
Patients must have the presence of parents or staff during the waiting period after application. Peroperative monitoring with blood pressure and ECG. The child may need a slightly extended wake-up time compared to patients without premedication.
Paracetamol
Given alone or in combination. Common combinations of pharmacological premedication for children usually include paracetamol (30 mg/kg x 1) in combination with benzodiazepines or benzodiazepine-like drugs, sometimes with the addition of an NSAID preparation. Paracetamol is given either as a tablet, mixture, orsuppository (Table 4). Children under 6 months are generally not premedicated. Several different drug combinations are common. Various types of sedative sympathomimetic drugs have become more common in recent times, such as clonidine and dexmedetomidine. These are usually given as an oral solution but can also be given intravenously.
A loading dose of paracetamol (max orally 30 mg/kg) is routinely given in premedication. It is practical to give a paracetamol mixture of 24 mg/ml, 1 ml/kg in the ward before most surgeries. Before more painful procedures, children > 6 months are also given an NSAID preparation. The youngest children, <6 months, are usually not premedicated.
Premedication and maintenance with paracetamol
Children 6-25 kg. Administered as a Mixture, Suppository or Tablet. | Premedication | Maintenance for the first 2 days 20 mg/kg body weight | |||||
|---|---|---|---|---|---|---|
| The child's weight (kg) | Mixture Paracetamol 24 mg/ml | Supp Paracetamol (mg) | Tablet Paracetamol (mg) | Mixture Paracetamol 24 mg/ml | Tablet Paracetamol (mg) | Supp Paracetamol (mg) |
| 6-8 kg | 8,5 ml | 250 mg | - | 2,5 ml x 4 | - | 60 mg x 4 |
| 8-10 kg | 12 ml | 310 mg | - | 3,5 ml x 4 | - | 125 mg x 3 |
| 10-12 kg | 14 ml | 375 mg | - | 5 ml x 3 | - | 125 mg x 4 |
| 12-15 kg | 17,5 ml | 500 mg | - | 5 ml x 4 | - | 185 mg x 4 |
| 15-20 kg | 22 ml | 625 mg | - | 7,5 ml x 4 | - | 250 mg x 3 |
| 20-25 kg | 28 ml | 750 mg | 500 mg | 10 ml x 4 | 500 mg x 3 | 250 mg x 4 |
Paracetamol Dosage for Children Orally o Rectally
| Loading dose | Maintenance dose | ||||
|---|---|---|---|---|---|
| Weight (kg) | Oral solution 24 mg/ml | Supp. | Weight (kg) | Oral solution 24 mg/ml | Supp. |
| 3 | 2,5 ml | S. 60 mg | 3 | 2,5 ml x 3 | S. 60 mg x 3 |
| 4 | 3,5 ml | S. 60 mg | 4 | 3,5 ml x 3 | S. 60 mg x 4 |
| 5 | 5 ml | S. 125 mg | 5 | 4 ml x 4 | S. 125 mg x 3 |
| 6 - 8 | 7 ml | S. 250 mg | 6 - 8 | 5 ml x 4 | S. 125 mg x 4 |
| 9 - 12 | 12 ml | S. 310 mg | 9 - 12 | 7,5 ml x 4 | S. 185 mg x 4 |
| 13 - 15 | 16 ml | 13 - 15 | 11 ml x 4 | ||
| Weight (kg) | Oral solution | Tablet | Weight (kg) | Oral solution | Tablet |
| 16 - 19 | 20 ml | T. 500 mg | 16 - 19 | 13 ml x 4 | T. 250 mg x 4 |
| 20 - 24 | 25 ml | T. 500 mg | 20 - 24 | 17 ml x 4 | T. 500 mg x 3 |
| 25 - 30 | 30 ml | T. 750 mg | 25 - 30 | 21 ml x 4 | T. 500 mg x 4 |
| 31 - 34 | 40 ml | T. 1000 mg | 31 - 34 | 25 ml x 4 | T. 750 mg x 3 |
| 35 - 42 | 40 ml | T. 1000 mg | 35 - 42 | 30 ml x 4 | T. 750 mg x 4 |
| 43 - 50 | 50 ml | T. 1250 mg | 43 - 50 | 35 ml x 4 | T. 1000 mg x 3 |
| 50 - 70 | 60 ml | T. 1500 mg | 50 - 70 | 40 ml x 4 | T. 1000 mg x 4 |
| >70 kg | 80 ml | T. 2000 mg | >70 kg | 40 ml x 4 | T. 1000 mg x 4 |
Paracetamol i v to Children
Paracetamol i v to Children. 10 mg/ml.| Weight (kg) | Dose |
|---|---|
| <1 months | 7,5 mg/kg |
| >1 months | 15 mg/kg |
| 4-10 kg | 6-15 ml x 4 |
| 10-20 kg | 15-30 ml x 4 |
| 20-33 kg | 30-50 ml x 4 |
| 33-50 kg | 50-75 ml x 4 |
| 50-66 kg | 75-100 ml x 4 |
| >66 kg | 100 ml x 4 |
Benzodiazepines
Given alone or in combination. A common standard mixture for children is midazolam + atropine in a mixture. This mixture is dosed according to a weight-based schedule. Midazolam often facilitates needle placement if EMLA has been used. Rectally, 0.3 mg/kg (max 10 mg) is given, as a nasal spray 0.2 mg/kg (max 5 mg), and orally 0.5 mg/kg (max 15 mg) can be given.
Midazolam Dosage for Sedation of Children
| Intravenously | Rectally | Nasally | Orally/PEG | |
|---|---|---|---|---|
| 0,1 mg/kg (max 5 mg) | 0,2-0,3 mg/kg (max 7,5-10 mg) | 0,2 mg/kg (max 5 mg) | 0,3-0,5 mg/kg (max 10-15 mg) | |
| An additional dose can be given according to the schedule below | ||||
| 0,05 mg/kg (after 5 minuter) | 0,05 mg/kg (after 20 minuter) | 0,05 mg/kg (after 10 min) | 0,05 mg/kg (after 20 min) | |
| At least one hour of monitoring after the last dose | At least one and a half hour of monitoring after the last dose | At least one hour of monitoring after the last dose |
Some children, such as those who are very anxious or have previously experienced significant problems with anesthesia, may be offered stronger premedication. Flunitrazepam in tablet form 0.05 mg/kg provides heavy sedation after about 20 minutes that lasts at least 1 hour. This premedication can be given in the ward, and the timing must be coordinated with the operating room. In some cases, midazolam can be given by anesthesia personnel to facilitate a difficult induction. The child must not be left alone after flunitrazepam or midazolam has been given. An alternative to midazolam is triazolam (Halcion). Dosage T. Halcion 0.125 mg, ½ tablet for children weighing 20-30 kg and 0.125 mg, 1 tablet for children weighing 30-40 kg. Older children may find the waiting time in the ward before surgery long and anxious. Diazepam (Stesolid), tablet or suppository, 0.5 mg/kg rounded down, max 25 mg rectally, can provide relief.
Atropine is given on medical order in the operating room, either intravenously, orally, subcutaneously, rectally, or sublingually.
Premedication with midazolam (children 10-25 kg)
A common standard mixture for children is midazolam + atropine in a mixture given orally. In addition, paracetamol 30 mg/kg x 1 is usually given.
Pharmacy mixture Midazolam 1 mg/ml + Atropine 0.05 mg/ml. Dosage: 0.4 mg (=0.4 ml)/kg according to the list below. The maximum dose for the mixture is 10 ml (orange flavor).
Midazolam 1 mg/ml + Atropine 0,05 mg/ml in a mixture
| Weight (kg) | Quantity in ml |
|---|---|
| 10 | 4,0 |
| 11 | 4,5 |
| 12 | 5,0 |
| 13 | 5,0 |
| 14 | 5,5 |
| 15 | 6,0 |
| 16 | 6,5 |
| 17 | 7,0 |
| 18 | 7,0 |
| 19 | 7,5 |
| 20 | 8,0 |
| 21 | 8,0 |
| 22 | 8,5 |
| 23 | 9,0 |
| 24 | 9,5 |
| 25 | 10,0 |
Premedication with midazolam (children 10-25 kg)
Midazolam + atropine in a mixture prepared in the operating room. Midazolam 1 mg/ml is mixed with Atropine 0.5 mg/ml, and strong juice is added to make a solution of 5–12 ml. Dosage: Midazolam 0.4 mg/kg + Atropine 0.02 mg/kg orally according to the list below. In addition, paracetamol 30 mg/kg x 1 is usually given.
Midazolam 1 mg/ml + Atropine 0,05 mg/ml
Mixed at op. dept. for children 10-25 kg. The dose is given orally in a mixture.| Weight (kg) | Volume in ml. of the mixture | Amount of medicine midazolam/atropine (mg) |
|---|---|---|
| 10 | 4,4 | 4,0/0,20 |
| 11 | 4,9 | 4,5/0,225 |
| 12 | 5,5 | 5,0/0,25 |
| 13 | 5,5 | 5,0/0,25 |
| 14 | 5,55 | 5,5/0,275 |
| 15 | 6,6 | 6,0/0,30 |
| 16 | 7,15 | 6,5/0,325 |
| 17 | 7,7 | 7,0/0,35 |
| 18 | 7,7 | 7,0/0,35 |
| 19 | 8,25 | 7,5/0,375 |
| 20 | 8,8 | 8,0/0,40 |
| 21 | 8,8 | 8,0/0,40 |
| 22 | 9,35 | 8,5/0,425 |
| 23 | 9,9 | 9,0/0,45 |
| 24 | 10,45 | 9,5/0,475 |
| 25 | 11 | 10,0/0,50 |
Premedication for rectal administration of midazolam (children 5-20 kg)
Midazolam + atropine in a mixture prepared in the operating room for rectal administration. Midazolam 5 mg/ml is mixed with 2 ml NaCl to a strength of 3 mg/ml. Dosage 0.3 mg/kg = 0.1 ml/kg. + Atropine 0.5 mg/ml is mixed undiluted in the midazolam mixture.
Rectal administration of Midazolam/Atropine to children 5-20 kg
| Weight (kg) | Midazolam 3 mg/ml Amount (mg) | Midazolam 3 mg/ml Volume (ml) | Atropine 0,5 mg/ml Amount (mg) | Atropine 0,5 mg/ml Volume (ml) |
|---|---|---|---|---|
| 5 | 1,5 | 0,5 | 0,15 | 0,3 |
| 7,5 | 2,25 | 0,75 | 0,15 | 0,3 |
| 10 | 3 | 1 | 0,15 | 0,3 |
| 12,5 | 3,75 | 1,25 | 0,25 | 0,5 |
| 15 | 4,5 | 1,5 | 0,25 | 0,5 |
| 20 | 6,0 | 2 | 0,25 | 0,5 |
Flumazenil for reversal of Bensodiazepines
| Flumazenil 0,1 mg/ml iv | Antidote for bensodiazepine overdose | ||||
|---|---|---|---|---|---|
| 5 µg/kg (0,05 ml/kg) intravenously once per minute up to 40 µg/kg (maximum dose 2 mg) | If lack of effect: continous infusion 2-10 µg/kg/hour |
Ketamine
Another option, especially for children with heart conditions aged 1-4 years, is ketamine 7 mg/kg mixed with midazolam 0.3 mg/kg. In cases where the child is not cooperative, ketamine can be given intramuscularly. A dose of 3-5 mg/kg is administered, in some cases up to 10 mg/kg, preferably in the deltoid muscle. If an injection is not desired and the child is uncooperative, ketamine can be given orally in exceptional cases. This induction method is time-consuming, about 20 minutes, until needle placement can occur. A dose of 6 mg/kg is given mixed with a small amount of liquid, such as Coca Cola.
Ketamin to children
| Ketamin (Ketalar®) | 10 mg/ml | 50 mg/ml |
|---|---|---|
| Iv bolus: | 0,5 mg/kg | Iv infusion 0,02-0,12 mg/kg/tim |
| Rectally | 4-5 mg/kg | |
| Esketamin (Ketanest®) | 5 mg/ml | 25 mg/ml |
| Rectally | 3 mg/kg | |
| Nasally | 1,5 mg/kg | |
| Should be combined with Midazolam or Dexmedetomidine! | ||
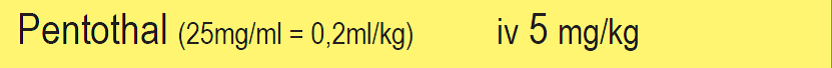
Thiopentone – Pentothal
Rectal induction with thiopentone (Pentocur – “Pentorect/Sleeping Tail”) can be given to small children aged 1-4 years (10-20 kg) if you prefer not to insert a needle while the child is awake. This is an older form of anesthesia that is hardly used anymore. Pentothal can be administered rectally at a dose of 30 mg/kg from a 100 mg/ml solution. This premedication acts as anesthesia induction and is administered in the operating room. The weight limits are not strict, and this induction often works well for sensitive children weighing 5-30 kg. The maximum rectal dose is 600 mg of Pentothal. Pentorect can be used as the sole form of anesthesia for minor surgical procedures or when you only want the child to remain still, such as during radiological examinations and certain radiological interventions.
Thiopentone for intravenous induction 25 mg/ml: 5 mg/kg iv 0.2 ml/kg
NSAID preparations that can be used for small children are Brufen mixture and Voltaren suppository
Premedication with mixture Ibuprofen (Brufen®) 20 mg/ml
Children 6-10 kg (> 6 months)| Weight (kg) | Dosage (ml) |
|---|---|
| 7 kg | 2,5 ml x 3 |
| 8 kg | 3,0 ml x 3 |
| 9 kg | 3,5 ml x 3 |
| 10 kg | 4,0 ml x 3 |
Ibuprofen for children (postoperatively)
| Ibuprofen | Oral suspension 20 mg/ml |
|---|---|
| ≥ 6 months 7,5 mg/kg x 4 alt. 10 mg/kg x 3 | Max 1200 mg/day |
| 0,375 ml/kg x 4 alt. 0,5 ml/kg x 3. | Max 60 ml/day |
Premedication with suppositories of diclofenac 25 mg
Children >1 year and >10 kg| Weight (kg) | Number of suppositories |
|---|---|
| 10 kg | ½ supp x 2 |
| 12,5 kg | ½ supp x 2 |
| 15 kg | ½ supp x 3 |
| 20 kg | 1 supp x 2 |
| 25 kg | 1 supp x 3 |
| 30-40 kg | 1½ supp x 3 |
Diclofenac to children (Voltaren®)
| Weight (kg) | Supp. | Tablet |
|---|---|---|
| 8-14 | 25 mg | 25 mg |
| 15-19 | 25+0+25 mg | 25+0+25 mg |
| 20-24 | 25+0+25 mg | 25+0+25 mg |
| 25-27 | 50+0+25 mg | 25+0+25 mg |
| 30-34 | 50+0+25 mg | 50+0+25 mg |
| 35-40 | 50+0+50 mg | 50+0+50 mg |
| 40-50 | 50+0+50 mg | 50+0+50 mg |
| >50 kg | 50+50+50 mg | 50+50+50 mg |

Practical advice before anesthesia for children
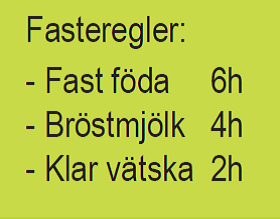
Fasting for children before anesthesia
- 2 hours fasting on clear liquids
- 6 hours fasting on everything other than clear liquids
- For infants under 6 months, 4 hours fasting on breast milk (and similar substitutes)
- Breastfeeding after 6 months – 4 or 6 hours fasting?
- Popsicles are not considered clear liquids
Some practical anesthesia routines
- One (1) parent follows the child into the operating room if the child is over 4 months old.
- Limit for outpatient care: 3 months of age (corrected age).
- Atropine only on indication
- Always use cuffed tubes
- Tube position (cm at the corner of the mouth) = patient height (cm)/10 + 5. Nasal: + 20%
- Propofol 5 mg/ml, lidocaine not needed
- Volume pumps (20 kg limit), no pediatric sets
- Often TIVA but never TCI < 16 years old
- Lots of EMLA, even for newborns.
Some common forms of anesthesia for children
- Induction: Propofol 5 mg/ml (as infusion 10 mg/ml); Pentothal 25 mg/ml (only in the heart room); Esketamine (different concentrations depending on the child’s size, often 1 or 5 mg/ml)
- Gas: Sevoflurane (mask induction, laryngeal mask). Isoflurane (heart anesthesia, neurosurgery). Desflurane (other intubation anesthesia).
- Opioid: Fentanyl 50 mcg/ml; Remifentanil 10 or 25 mcg/ml. Alfentanil is not routinely used. Morphine is available.
- Relaxant: Rocuronium 10 mg/ml. (Celokurin 50 mg/ml is always drawn up, as well as atropine)
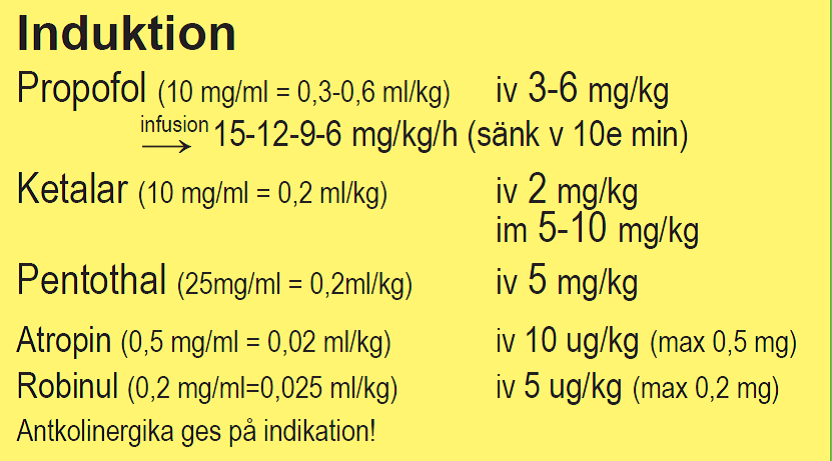
Anesthesia Induction
- Propofol 3-6 mg/kg iv (10 mg/ml = 0.3-0.6 ml/kg)
- Propofol in infusion 15-12-9-6 mg/kg/h (reduce every 10 minutes)
- Ketamine (Ketalar) 2 mg/kg iv (10 mg/ml = 0.2 ml/kg)
- + Midazolam 0.1-0.3 mg/kg iv (5-10 mg/kg im)
- Pentothal 4-5 mg/kg iv (25 mg/ml = 0.2 ml/kg)
- Atropine 10 μg/kg (max 0.5 mg) iv (0.5 mg/ml = 0.02 ml/kg)
- Robinul 5 μg/kg (max 0.2 mg) iv (0.2 mg/ml=0.025 ml/kg)
Anticholinergics are given only on indication!

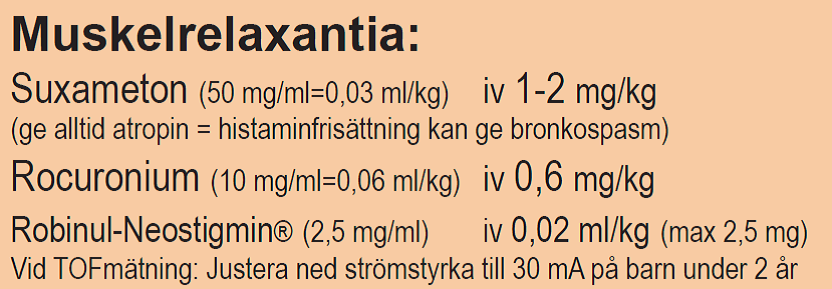
Muscle Relaxants
- Suxamethonium (Celokurin®) 1-2 mg/kg iv (50 mg/ml=0.03 ml/kg). Always give atropine in advance = histamine release can cause bronchospasm
- Rocuronium 0.6 mg/kg iv (10 mg/ml=0.06 ml/kg)
- Robinul-Neostigmine® 0.02 ml/kg iv (max 2.5 mg) (2.5 mg/ml)
- With TOF measurement: Adjust the current down to 25 mA for children under 2 years
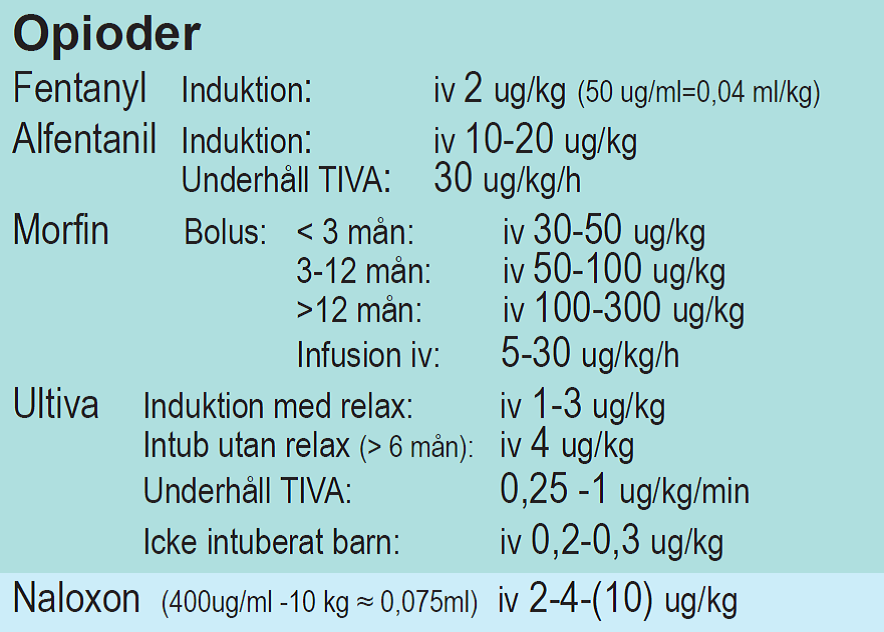
Opioids
- Fentanyl
- Induction: iv 2 μg/kg (50 μg/ml=0.04 ml/kg)
- Alfentanil
- Induction: iv 10-20 μg/kg
- Maintenance TIVA: 30 μg/kg/h
- Morphine
- Bolus: < 3 months: iv 30-50 μg/kg
- 3-12 months: iv 50-100 μg/kg
- > 12 months: iv 100-200-(300) μg/kg
- Infusion iv: 5-30 μg/kg/h
- Remifentanil (Ultiva)
- Induction with relax: iv 1-3 μg/kg
- Intubation without relax (> 6 months): iv 4 μg/kg
- Maintenance TIVA: 0.25-1 μg/kg/min
- Non-intubated child: iv 0.2-0.3 μg/kg
- Naloxone
- (400 μg/ml -10 kg ≈ 0.075 ml) iv 2-4-(10) μg/kg
Oxicodon for children (postoperative pain treatment)
| Oxicodon (Oxynorm) | 1 mg/ml |
|---|---|
| Oral solution | 0.1-0.2 mg/kg (max. 10 mg) up to 4 times/day |
| Given for severe opioid-sensitive pain. | ATTENTION! At least one hour of monitoring after the last dose! |
Fentanyl for children
| Fentanyl | 50 µg/ml (0.05 mg/ml) |
|---|---|
| Intravenously | 1 µg/kg |
| In continuous infusion for sedation in the ICU | 0,5-1 μg/kg/hour |
| Nasally | > 3 years 1,5 µg/kg |
Intravenous naloxone dosage for children (Nexodal®)
| Naloxone iv | Dosage 2 µg/kg | The dose can be repeated if necessary |
|---|---|---|
| Weight (kg) | Solution 20 µg/ml | Solution 0.4 mg/ml (children > 20 kg) |
| 3-5 kg | 0,3-0,5 ml | |
| 5-10 kg | 0,5-1,0 ml | |
| 10-20 kg | 1,0-2,0 ml | |
| 20-40 kg | 2,0-4,0 ml | 0,1-0,2 ml |
| 40-80 kg | 4,0-8,0 ml | 0,2-0,4 ml |
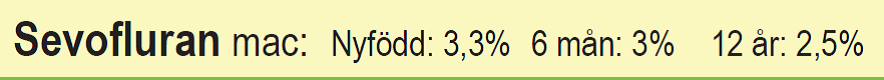
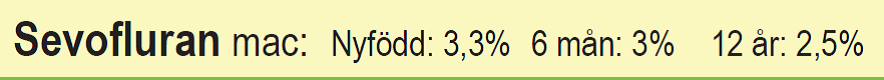
MAC values for Sevoflurane
- Newborn: 3.3%
- 6 months: 3%
- 12 years: 2.5%

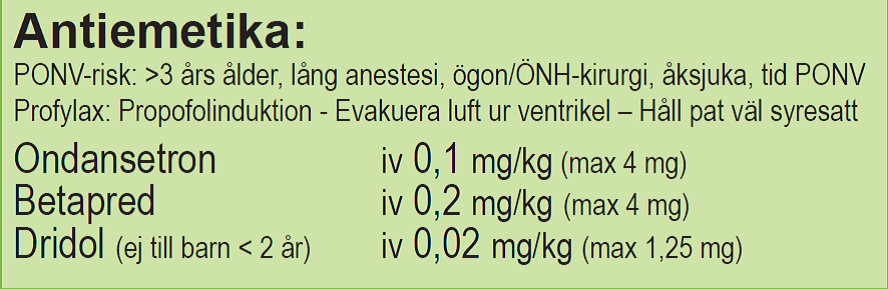
Antiemetics
- PONV risk: > 3 years old, long anesthesia, eye/ENT surgery, motion sickness, previous PONV
- Prophylaxis: Propofol induction – Evacuate air from the stomach – Keep the patient well oxygenated
- Ondansetron iv 0.1 mg/kg (max 4 mg)
- Betamethasone iv 0.2 mg/kg (max 4 mg)
- Dridol (not for children < 2 years) iv 0.02 mg/kg (max 1.25 mg)
Peripheral analgesics
- Ketorolac (Toradol®) 0.3 mg/kg x 4 iv (not < 3-6 months, COX 1+2)
- Parecoxib (Dynastat®) 0.5 mg/kg x 1 iv (not < 3-6 months COX 2)
- Ibuprofen 7.5 mg/kg x 3-4 po (not < 3 months COX 1+2)
- Paracetamol po 15 mg/kg x 4 (first 3 days 20-25 mg/kg x 4)
- Paracetamol iv 15 mg/kg x 4 (use iv mainly on the first postoperative day)

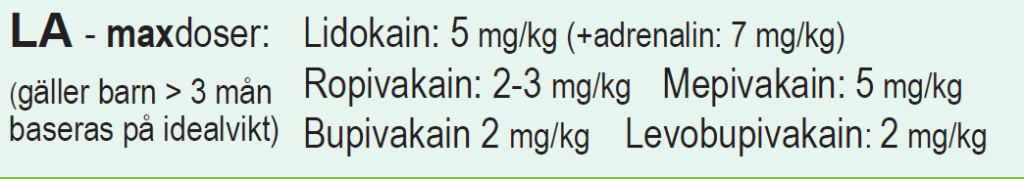
Maximum doses of local anesthetics for children
- Lidocaine: 5 mg/kg
- Lidocaine + adrenaline: 7 mg/kg
- Ropivacaine: 2-3 mg/kg
- Mepivacaine: 5 mg/kg
- Bupivacaine 2 mg/kg
- Levobupivacaine: 2 mg/kg
Applies to children > 3 months. Based on ideal weight
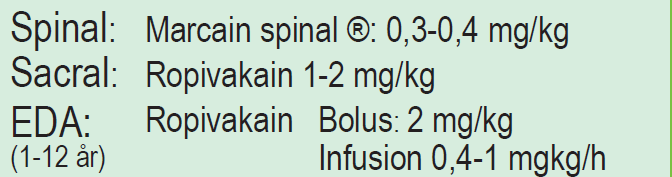
Regional anesthesia
- Spinal: Marcain spinal®: 0.3-0.4 mg/kg
- Sacral: Ropivacaine 1-2 mg/kg
- EDA (1-12 years): Ropivacaine (Narop)
- Bolus: 2 mg/kg
- Infusion 0.4-1 mg/kg/h
Size of endotracheal tubes for children
| Age | 0 | 3 months | 1 year | 5 years | 9 years | 12 years | 14 years | > 15 years |
|---|---|---|---|---|---|---|---|---|
| Weight | 3 kg | 5 kg | 10 kg | 20 kg | 30 kg | 40 kg | 50 kg | > 50 kg |
| Endotracheal tube internal diameter (mm) | 3 | 3.5 | 4 | 5 | 6 | 7 | 7 | 7 |
CVC sizes for children
| Weight | CVL Sizes | Catheter length |
|---|---|---|
| <10 kg | 3–5 French | 4–6 cm |
| 10–30 kg | 5–6 French | 6–8 cm |
| >30 kg | 7 French | 10–15 cm |
Laryngeal mask for children
| LMA Size | Patient Size | Cuff Volume (mL) | Max ETT Diameter |
|---|---|---|---|
| 1 | < 5 kg | 4 mL | 3.5 |
| 1.5 | 5–10 kg | 7 mL | 4 |
| 2 | 10–20 kg | 10 mL | 4.5 |
| 2.5 | 20–30 kg | 14 mL | 5 |
| 3 | 30–50 kg | 20 mL | 6 |
| 4 | 50–70 kg | 30 mL | 6 |
| 5 | 70–100 kg | 40 mL | 7 |
Laryngoscope / Blade Size for children
| Age | Macintosh | Miller |
|---|---|---|
| Very preterm | n/a | 00 |
| Preterm | 0 | 0 |
| Neonate / small infant | 0 | 0 |
| Infant to 2 years of age | 1 | 1 |
| 2–8 years of age | 2 | 2 |

Normal height and weight in children
| Age | Height (cm) | Weight (kg) |
|---|---|---|
| Newborn | 50 | 3,5 |
| 3 months | 60 | 6 |
| 1 year | 75 | 10 |
| 3 years | 95 | 15 |
| 7 years | 120 | 25 |
| 10 years | 140 | 30 |
Normal Reference Values for Children
| Age | Pulse hr/min | Blood pressure syst/dia | Respiratory Rate | Blood Volume | Hgb-values (g/l) |
|---|---|---|---|---|---|
| Newborn | 100-180 | 60/35 (MAP 40-45) | 40-60 | 85 ml/kg | 150-180 |
| 0-6 months | 100-160 | 60-90/30-60 | 30-60 | 85 ml/kg | 90-100 |
| 6-12 months | 100-160 | 80-95/45-65 | 25-50 | 85 ml/kg | 100 |
| 1-2 years old | 100-150 | 85-105/55-65 | 25-35 | 80 ml/kg | 100 |
| Preschool | 70-110 | 95-105/55-65 | 20-35 | 75 ml/kg | 100-110 |
| School age (7-12) | 65-110 | 95-115/55-70 | 18-30 | 75 ml/kg | 110-120 |
| Teen Age | 60-90 | 110-130/65-80 | 12-16 | 75 ml/kg | 120-130 |
Pediatric Anesthesia Pocket Guide
TIVA for pediatric anesthesia
Job Description
- Fixed placement of syringe pumps with medications: remifentanil at the top and propofol at the bottom.
- The syringe pump with remifentanil should be set to micrograms/kg/minute.
- The syringe pump with propofol should be set to mg/kg/hour.
- Back valve for the infusion with remifentanil.
- Avoid using the blood pressure cuff on the same arm.
Initiating Anesthesia
Pre-oxygenation is given with 80% oxygen. The patient is ventilated with a breathing mask and breathing bag until the patient is ready for laryngeal mask placement or intubation.
- Bolus propofol 5 mg/ml (“pediatric propofol”) 3 – 6 mg/kg iv.
- Bolus fentanyl 1 – 3 micrograms/kg iv during induction.
- Start the infusion with remifentanil 0.5 micrograms/kg/min once the child is asleep.
- Atropine 0.01 mg/kg iv is only given on indication.
If anesthesia begins with sevoflurane inhalation (e.g., when a venous cannula is missing), it can be converted to TIVA after the child is asleep. Half of the bolus dose of propofol is then given, and other medications according to previous protocol.
Intubation
- Minimize the use of muscle relaxants.
- Remifentanil 4 micrograms/kg usually provides good intubation conditions in combination with
- Propofol 3.5 mg/kg
- Note! Do not intubate when the vocal cords are centered! This can damage the vocal cords.
Maintenance
- Remifentanil 0.5 – 1.0 micrograms/kg/min
- Propofol 8 – 12 mg/kg/h, which can gradually be reduced to 6 mg/kg/h.
The doses are adjusted according to the clinic.
Conclusion
Propofol and remifentanil infusions are stopped when nearing the end of the surgery.
Remember to give a bolus of fentanyl 1 – 2 micrograms/kg iv for postoperative pain relief.
The ventilator continues to operate until the patient wakes up and can be extubated or the laryngeal mask can be removed.
Local Anesthesia
Good local/regional anesthesia should be provided to as many patients as possible. For skin closure of surgical wounds, local wound infiltration can be given with bupivacaine 2.5 mg/kg 0.5 ml/kg.
Medication Mixing
- Remifentanil 50 micrograms/ml: 2 mg remifentanil dissolved in 40 ml 0.9% NaCl.
- Propofol is given at a concentration of 5 mg/ml
References
- Solheim A, Raeder J. Remifentanil versus fentanyl for propofol-based anesthesia in ambulatory surgery in children. Ambulatory Surgery. March 2011; 17 – 20.
- Klemola UM, Hiller A. Tracheal intubation after induction of anesthesia in children with propofol – remifentanil or propofol rocuronium. Can J Anaesth. September 2000, 47 (9): 854 – 9.
- Procedures from Ahus: “Anesthesia for children – TIVA in patients under 16 years”, version 1.4, date 24.01.2014.
Circulation hemodynamics
- There is no good data on blood pressure limits for children (partly because complications are rare)
- Circulation and perfusion should be assessed using multiple modalities (lactate, urine output, etc.)
- You have to manage without PA catheters and most other invasive CO measurements
- NIRS is widely used
- Don’t forget capillary refill! Most useful in emergencies (can be used to estimate CO, but not SVR)
Rules of thumb for perioperative MAP
- Premature or newborn: MAP ≥ gestational weeks
- Up to one year of age: MAP ≥ 45 mm Hg
- 1-5 years: MAP ≥ 50 mm Hg
- 5 years and up: MAP ≥ 50-60 mm Hg
Target values for blood pressure in children under general anesthesia (Mean arterial pressure - MAP in mmHg)
| Age | Anesthetized | Awake |
|---|---|---|
| 0-3 months | 42-47 | 52 |
| 3-6 months | 45-52 | 57 |
| 6-12 months | 51-57 | 63 |
| 1-3 years | 51-57 | 63 |
| 3-6 years | 54-61 | 68 |
| 6-14 years | 58-65 | 70 |
| > 14 years | 58-65 | 73 |
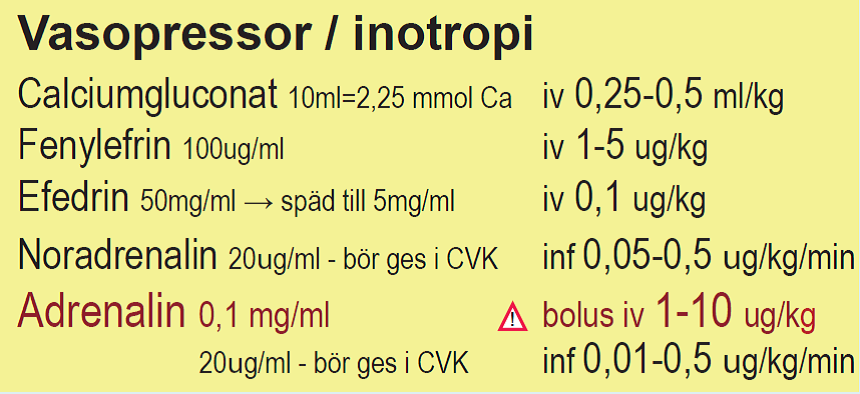
Blood pressure-raising and inotropic drugs
- The same drugs can be used as for adults
- Norepinephrine is usually the first choice, starting dose 25-100 ng/kg/min
- Adrenaline can be given as inotropy, 10-30 ng/kg/min
- Dopamine is an alternative, 5-20 ng/kg/min
- Milrinone for inotropy + afterload reduction, 0.3-0.7 μg/kg/min
- Ca2+ infusion can be used if S-Ca is low
Vasopressor/Inotropy
- Calcium gluconate 10 ml = 2.25 mmol Ca2+: 0.25-0.5 ml/kg iv
- Phenylephrine 100 μg/ml, 1-5 μg/kg iv
- Ephedrine 50 mg/ml → dilute to 5 mg/ml: 0.1 mg/kg iv
- Norepinephrine 20 μg/ml – should be given in continuous infusion in CVK: 0.05-0.5 μg/kg/min iv
- Adrenaline 0.1 mg/ml: in bolus doses: 0.1→1→10 μg/kg iv
- Adrenaline in continuous infusion 20 μg/ml – should be given in CVK: 0.01-0.5 μg/kg/min iv
MAC values for children during inhalation anesthesia
| Patient's age (years) | Sevoflurane in oxygen (%) | Sevoflurane in 65% N2O/ 35% O2 |
|---|---|---|
| 0 - 1 months * | 3.3% | Not determined |
| 1 - <6 months | 3.0% | Not determined |
| 6 months - <3 years | 2.8% | 2,0 %** |
| 3 to 12 years | 2.5% | Not determined |
| 25 years | 2.6% | 1.4% |
| 40 years | 2.1% | 1.1% |
| 60 years | 1.7% | 0.9% |
| 80 years | 1.4% | 0.7% |
| *Newborn children after full term pregnancy. MAC in premature infants has yet to be determined. | ||
| **In pediatric patients 1-<3 years old, 60% N2O/40% O2 was used. | ||
Laryngospasm in children
Risk factors
- Upper respiratory infection (recent viral illness)
- fever
- productive cough
- colored mucus secretion within 2 weeks
- Asthma
- Whooping cough within 6 months
- RS virus
- Young age
- ENT surgery
- Airway manipulations
- Mucus secretion in the airways or bleeding
Prophylaxis
- Consider postponing the surgery if possible
- IV induction
- Nasal decongestant drops (“Nezeril”)
- Anticholinergics; Glycopyrronium (
Robinul) or Atropine iv. - Extubation in the lateral position
- Small doses of propofol at awakening and extubation
- Avoid mucus from the airways or bleeding
- Lidocaine iv 1 mg/kg
- Racepinephrine (racemic adrenaline)
Measures and treatment
- Remove the triggering stimuli
- Jaw thrust
- 100% O2 with mask
- Call a colleague (ask for assistance)
- Manual mask ventilation + PEEP
- Muscle relaxation in severe cases – saturation below 90% (subclinical dose of suxamethonium may be sufficient)
- Atropine to avoid bradycardia and hypotension
- Intubation in case of unsatisfactory airway
- CPR as a last resort
If an intravenous line is available
- Propofol 0.5-3.0 mg/kg
- Suxamethonium (Celokurin) 0.25-2 mg/kg (subclinical dose may be sufficient)
- + Atropine 10 micrograms/kg for high doses of suxamethonium
If an intravenous line is not available
- Consider intraosseous needle!
- i.o. Suxamethonium 4 mg/kg
Fluid therapy for children
- Albumin 5% is the standard for volume needs
- Ringer-Acetate works in most situations
- Blood, platelets, etc., based on need
- Everything can be given in boluses of 10 ml/kg over 1-4 hours
- If in a hurry, it’s easiest to give volume directly with a syringe (goes quickly for small children < 10 kg)
- Hgb limits are debated for heart-healthy children but should cope with Hgb 8-9 g/dL
Clinical signs of dehydration in Children
| Symptoms / signs | Mild | Moderate | Severe |
|---|---|---|---|
| Weight loss | < 5 % | 5–10 % | > 10 % |
| Deficit (ml/kg) | < 50 | 50–100 | > 100 |
| General condition | Thirsty and worried | Thirsty, anxious or lethargic, halonated | Very sluggish to comatose, cold, gray, cyanotic |
| Mucous membranes | Normal, moisty | Dry | Very dry |
| Skin turgor | Normal | Reduced | Pronounced impaired |
| Fontanelle | Normal | Sunken | Very sunken |
| Pulse | Normal | Tachycardia | Tachycardia, weak pulse |
| Capillary refill | < 2 sec | Slow > 2 sec | Very slow |
| Blood pressure (systolic) | Normal | Normal / low | Low |
| Breathing | Normal | Deep | Deep and fast |
| Diuresis (urinary output) | < 2 ml/kg/h | < 1 ml/kg/h | < 0,5 ml/kg/h |
| NOTE! Higher dehydration can be used without all the characters being met. In hyperosmolar conditions with dehydration, the symptoms may appear different. Drops in blood pressure will often be late and are ominous. | |||
Fluid therapy in dehydration
| Percentual deficit of total body weight | Symptom | Exampel at body weight 70 kg | 4 hours (2/3 of need) |
|---|---|---|---|
| Two percent deficit | Dry mucous membranes, thirst | 1,4 liter | 0,9 liter |
| Five percent deficit | Tachycardia, pronounced thirst, oliguria | 3,5 liter | 2,3 liter |
| Ten percent deficit | Hypotension, vasoconstriction, cognitive impairment, pronounced orthostatism | 7 liter | 5 liter |
Baseline fluid requirements (Use the 4/2/1 rule)
- 0 – 10 kg → 4 ml/kg/hour
- 10 – 20 kg → 40 ml/hour + 2 ml/kg/hour for weight > 10 kg
- > 20 kg → 60 ml/hour + 1 ml/kg/hour for weight > 20 kg
Preoperative supply of maintenance fluid volume
| Patient weight | Volume requirement according to Holliday and Segar/day | Example basal supply (ml/day) | Preoperative maintenance fluid (ml/day) |
|---|---|---|---|
| ≤ 10 kg | 100 ml/kg | 8 kg 8 × 100 = 800 | 800 × 0,8 = 640 |
| 10–20 kg | 1,000 ml + 50 ml/kg for every kg over 10 kg | 15 kg 1 000 + 5 × 50 = 1 250 | 1 250 × 0,8 = 1 000 |
| ≥ 20 kg | 1,500 ml + 20 ml/kg for every kg over 20 kg | 25 kg 1 500 + 5 × 20 = 1 600 | 1 600 × 0,8 = 1 280 |
Perioperative fluid requirements (Ringer-Acetate = standard)
- Children < 10 kg: 10 ml/kg/hour for the first 1-2 hours
- Children > 10 kg: 3 – 5 ml/kg/hour for the first 1-2 hours
- Then 1-2 ml/kg/hour + measured/estimated losses
- 3rd space loss: 1-10 ml/kg/hour depending on the type of surgery
Peroperative fluid requirement
| Patient weight | Basic volume requirement | After 1-2 hours | Add for 3rd room loss: |
|---|---|---|---|
| ≤ 10 kg | 10 ml/kg first 1-2 hours | 1-2 ml/kg/h + measured/estimated losses | 1-10 ml/kg/h depending on type of surgery |
| 10–20 kg | 3-5 ml/kg first 1-2 hours | 1-2 ml/kg/h + measured/estimated losses | 1-2 ml/kg/h + measured/estimated losses |
| ≥ 20 kg | 3-5 ml/kg first 1-2 hours | 1-2 ml/kg/h + measured/estimated losses | 1-2 ml/kg/h + measured/estimated losses |
If bolus doses of fluid are needed
- Ringer-Acetate: 5 – 10 – 20 ml/kg
- Albumin 5% 5 – 10 – 20 ml/kg
- Blood products: 5 – 10 – 20 ml/kg
Bolus doses of fluids for children
| Type of infusion | Volume | Magnitude of volume loss |
|---|---|---|
| Cristalloid | 10-20 ml/kg | At 5-10% volume loss |
| Albumin 5% | 5-10 ml/kg | At 10-20% volume loss |
| Blood | 10-20 ml/kg | At >20% blood loss according to Hb |
| Plasma | 10-20 ml/kg | At >50% blood loss according to ROTEM |
Recommendations for children with major bleeding
- Red blood cell concentrate 10 ml/kg in repeated doses
- Plasma 10–20 ml/kg
- Platelet concentrate 5–10 ml/kg
- Cryoprecipitate 5 ml/kg
- Fibrinogen concentrate 30 mg/kg
- Tranexamic acid 10–15 mg/kg
- Recombinant factor VIIa 90 μg/kg
Perioperative glucose supply
- Glucose 10% + 40 Na/20 K
- 3 ml/kg/h → adjust according to blood glucose!
- Indications
- Children < 1 week old if there is ongoing glucose infusion preoperatively
- Metabolic disease
- Growth-retarded newborns
Postoperative fluid requirements
- Give 75% of the 4/2/1 rule on the first postoperative day (due to elevated ADH)
- Ringer-Acetate
- Glucose 10% + 120 Na/20 K (Reduce electrolytes for children < 6 months)
Volume of postoperative maintenance fluid
| Patient weight | Basal volume requirement, /day | Example basal supply (ml/day) | After postoperative reduction (ml/day) |
|---|---|---|---|
| ≤ 10 kg | 100 ml/kg | 8 kg 8 × 100 = 800 | 800 × 0,7 = 560 |
| 10–20 kg | 1,000 ml + 50 ml/kg for every kg over 10 kg | 15 kg 1 000 + 5 × 50 = 1 250 | 1 250 × 0,7 = 875 |
| ≥ 20 kg | 1,500 ml + 20 ml/kg for every kg over 20 kg | 25 kg 1 500 + 5 x 20 = 1 600 | 1 600 × 0,7 = 1 120 |
Electrolyte content in losses of various body fluids in mmoll
| Body fluid | Na (mmol/l) | K (mmol/l) | Cl (mmol/l) | HCO3 (mmol/l) | H (mmol/l) |
|---|---|---|---|---|---|
| Stomach (Gastric content) | 20–60 | 14 | 140 | 60–80 | |
| Bile | 145 | 5 | 105 | 30 | |
| Diarrhea / colostomy losses | 30–140 | 30–70 | 20–80 | ||
| Losses from the ileum at high flows | 100–140 | 4–5 | 75–125 | 0–30 | |
| Losses from the ileum at low flows | 50–100 | 4–5 | 25–75 | 0–30 | |
| Drainage or fistula from the pancreas | 125–138 | 8 | 56 | 85 | |
| Losses from the jejunum | 140 | 5 | 135 | 8 | |
| Polyuria | Varies | Varies | |||
| Ref: Neilson J, O’Neill F, Dawoud D, Crean P, Guideline Development G. Intravenous fluids in children and young people: summary of NICE guidance. BMJ (Clinical research ed). 2015;351:h6388 | |||||
Total intravenous fluid supply to be assumed during the first days of life
| Age | Volume |
|---|---|
| Day of life 1 | 60–70 ml/kg/day |
| Day of life 2 | 70–80 ml/kg/day |
| Day of life 3 | 80–100 ml/kg/day |
| From four days old | 100 ml/kg/day |
Estimated fluid needs for intravenous maintenance treatment of children and adolescents
| Weight | Daily fluid needs(ml/24 h) | Fluid demand per hour (ml/h) |
|---|---|---|
| < 10 kg | 100 ml/kg/24 hours | 4 ml/kg/h |
| 10–20 kg | 1,000 ml + (50 ml/kg/24 h for each kg more than 10 kg) | 40 ml/h + (2 ml/kg/h for each kg more than 10 kg) |
| > 20 kg | 1 500 ml + (20 ml/kg/24 tim för varje kg över 20 kg*) | 60 ml/tim + (1 ml/kg/tim för varje kg över 20 kg)* |
| * Girls rarely need more than 2,000 ml / day and boys rarely need more than 2,500 ml / day as maintenance treatment even at weights exceeding 45 and 70 kg respectively. | ||
The child's total fluid needs
Fluid requirements per kg of body weight (Holliday-Segar)| Weight (kg) | Quantity per day |
|---|---|
| Children born before w.37 and during the neonatal period | See PM for patients at Neonatal |
| < 5 kg | 150 ml/kg |
| 5 -10 kg | 100 ml/kg |
| 11 - 20 kg | 1000 ml + 50 ml for every kg over 10 kg |
| > 20 | 1500 ml + 20 ml for every kg over 20 kg |
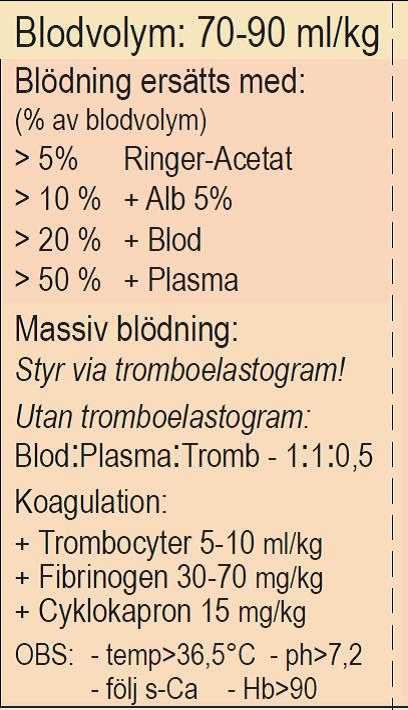
Bleeding
Blood volume: 70-90 ml/kg
Bleeding is compensated according to volume loss as a percentage of blood volume
- 5-10 % Ringer’s Acetate
- > 10 % + Albumin 5%
- > 20 % + Blood
- > 50 % + Plasma
Massive Bleeding
- Monitor via thromboelastogram!
- Without thromboelastogram:
- Give Blood/Plasma/Platelets in the ratio: 1:1:0.5
If Coagulation Disorder
- + Platelets 5-10 ml/kg
- + Fibrinogen 30-70 mg/kg
- + Tranexamic Acid 15 mg/kg
Note
- Temperature > 36.5°C
- pH > 7.2
- Monitor s-Ca
- Hgb > 9 g/dL
Regional Anesthesia for Children
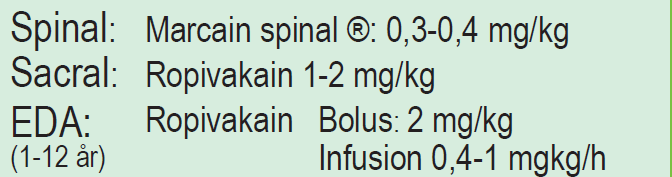
Regional Anesthesia
- Spinal: Marcain spinal®: 0.3-0.4 mg/kg
- Sacral: Ropivacaine 1-2 mg/kg
- EDA (1-12 years): Ropivacaine (Narop®)
- Bolus: 2 mg/kg
- Infusion 0.4-1 mg/kg/h
Mechanical Ventilation of Children
- Smaller lung volume/kg, larger anatomical dead space, and greater work of breathing than adults
- Higher metabolism = higher O2 consumption
- Normal expiration at rest causes the lung to fall below its closing capacity
- Lack of bronchioalveolar connections (increased risk of atelectasis)
- Small children desaturate quickly during apnea
- Pre-oxygenation can be difficult during induction
- There is often no time to search for the right tools when things get serious…
Ventilation – Ventilator Settings
- Usually pressure-controlled ventilation for children (PC, PRVC, or SIMV+PC is common modes)
- Tidal volume usually 6-7 ml/kg, PEEP 5 as standard (sometimes higher)
- Preferably FiO2 < 0.5
- Recruitments can (and should) be done as usual but often do not yield as good results as in adults
- How much leakage can be tolerated from an uncuffed tube is a debated issue…
- NAVA ventilation is sometimes used (perhaps too rarely)
NIV
- Can be operated with a full mask, nasal mask, “dummy plug,” or nasal tube
- Full mask works best for larger children, nasal mask, or dummy plug for small children
- Nasal tube can work but often bothers patients => lots of agitation and poor breathing best conditions if the patient goes from nasal intubation to NIV
- NIV has become rare in pediatric ICU after the arrival of high-flow nasal cannulas
- Requires competent staff to function
Ventilation – Tips Before Extubation
- Small children must be quite awake to avoid apnea after extubation
- Preferably PEEP 5 and PC 5-7, FiO2 < 0.35
- Suction the throat and open nostrils, give nasal drops if needed
- Solu Cortef 5 mg/kg (max 100 mg) can be given when the patient has been on a ventilator for a few days
- Micronefrin (racemic adrenaline) in nebulizer is good for small children as a decongestant in the upper airways, 0.05 ml/kg, max 0.75 ml (not in tube or tight mask)
- High-flow nasal cannula is very useful if you think it will be tough for the patient after extubation
Difficult Airway Management


Sedation of Children on a Ventilator
Goal
- Calm children without stress or pain
- They can be fully awake if they tolerate it
- Smaller children often tolerate being awake with the tube much better than adults
- It’s important to explain the goal to the parents
- Pain can be difficult to interpret (e.g., stomach cramps)
- Convince colleagues in surgery to place an EDA as often as possible (greatly simplifies things)
Treatment
- Morphine is the standard treatment for analgesia (normally up to 30 µg/kg/h)
- Rotation to ketobemidone or oxycodone can be done after one week
- Dexmedetomidine is now the first choice for sedation, normally 0.4-1.4 µg/kg/h (Children < 3 months should probably max at 1.0 µg/kg/h)
- Propofol can be used, preferably not for children < 1 year and preferably not > 4 mg/kg/h, but it facilitates extubation of larger children
- Phenobarbital is a good complement that rarely affects breathing or circulation; 5 mg/kg, max 3 times/day can be given
Strategy for Extubation
- Reduce opioid administration to the lowest level you think is needed, preferably the day before
- Supplement with paracetamol
- Reduce dexmedetomidine to 0.4-0.8 µg/kg/h, switch to propofol or combine them
- If midazolam is used, discontinue it early in the morning (a task for the on-call staff)
- When the ventilator settings allow it, turn off propofol, keep some dexmedetomidine if ongoing, and wait for the patient to wake up
- Larger patients can be extubated with a bit of propofol remaining (1-2 mg/kg/h) for a calmer awakening
Sedation by infusion for children on a Ventilator
| Drug | Infusion dose | Concentration | Caution |
|---|---|---|---|
| Dexmedetomidine | 0,4 - 1,4 μg/kg/h | < 15 kg 4 μg/ml > 15 kg 8 μg/ml | Starting dose usually 0.7 μg/kg/h. Never give bolus. Treatment time max 2 weeks. Caution bradycardia, hyperthermia |
| Clonidine | 0,5 - 2 μg/kg/h | 15 μg/ml | |
| Midazolam | 0,05 - 0,2 mg/kg/h | < 15 kg 1 mg/ml > 15 kg 5 mg/ml | Bolus: 0,05-0,1 mg/kg |
| Morphine | 5 - 30 μg/kg/h | < 15 kg 0,1 mg/ml > 15 kg 1 mg/ml | Bolus: 0,05-0,1 mg/kg |
| Propolipid | 1 - 4 mg/kg/h | 20 mg/ml | Children > 3 years. Bolus: 1-3 mg/kg |
| Fentanyl | 0,5 - 1 μg/kg/h | 50 μg/ml | Higher doses may need to be given. Max 6 μg/kg/h. |
Optiflow (High-Flow Nasal Cannula) for Children
The flows in high-flow nasal cannula (HFNC/"Optiflow") for children
| Weight | Flow (l/min) |
|---|---|
| 2-6 kg | The child's weight + 1 l/min up to 2 l/min/kg |
| 7-9 kg | The child's weight + 1-2 l/min |
| 10-14 kg | Start at 10 l/min, increase as needed to 15 l/min |
| 15-19 kg | Start at 15 l/min, increase as needed to 20 l/min |
| 20-49 kg | 20-25 l/min |
| >50 kg | 25 l/min up to 40 l/min |
Resuscitation of Children

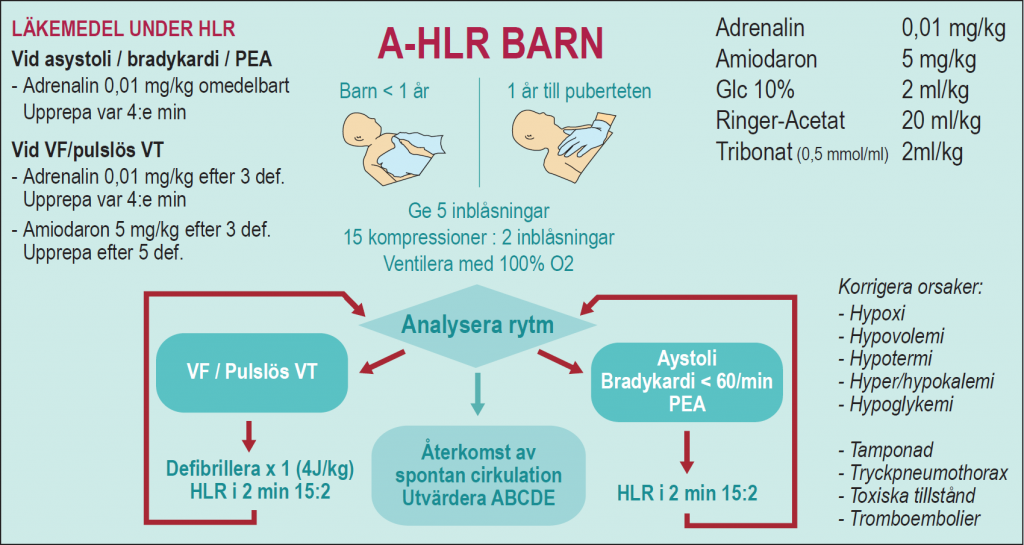
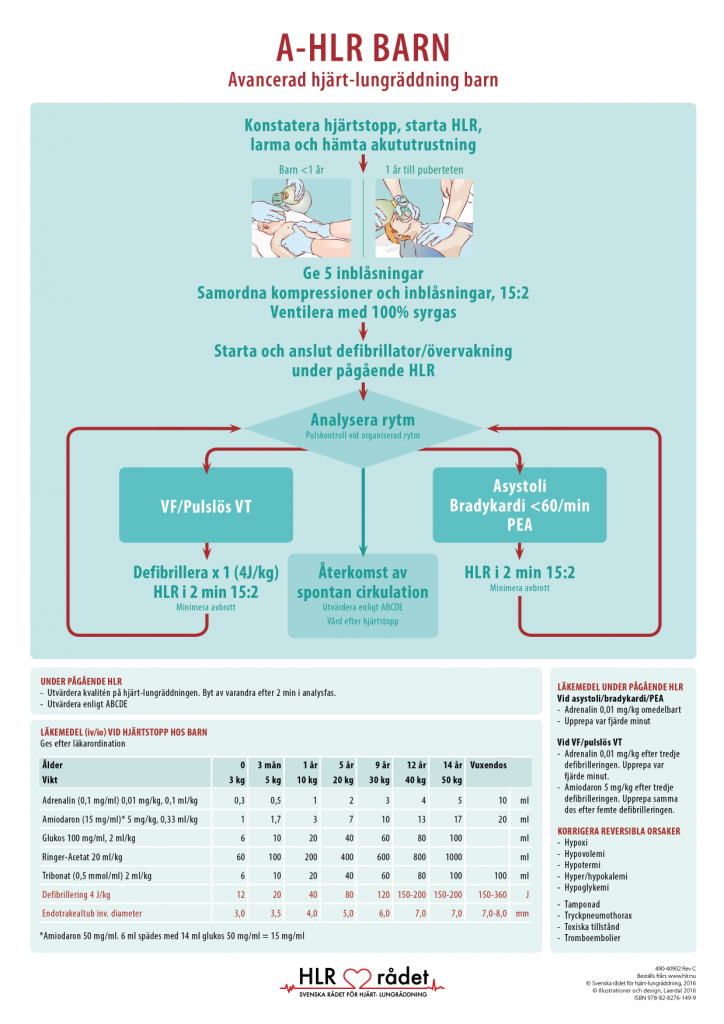
Medications During Ongoing Pediatric CPR
In cases of asystole/bradycardia/PEA
- Adrenaline 0.01 mg/kg immediately
- Repeat every four minutes
Medications at cardiac arrest in children
| Age | 0 | 3 months | 1 year | 5 years | 9 years | 12 years | 14 years | 15 years and older | |
|---|---|---|---|---|---|---|---|---|---|
| Weight | 3 kg | 5 kg | 10 kg | 20 kg | 30 kg | 40 kg | 50 kg | > 50 kg | |
| Epinephrine (0,1 mg/ml)* 0,01 mg/kg, 0,1 ml/kg | 0.3 | 0.5 | 1 | 2 | 3 | 4 | 5 | 10 | ml |
| Amiodarone (15 mg/ml)* 5 mg/kg, 0,33 ml/kg | 1 | 1.7 | 3 | 7 | 10 | 13 | 17 | 20 | ml |
| Glucose 100 mg/ml, 2 ml/kg | 6 | 10 | 20 | 40 | 60 | 80 | 100 | ml | |
| Ringer's Acetate 20 ml/kg | 60 | 100 | 200 | 400 | 600 | 800 | 1000 | ml | |
| Tribonate (0,5 mmol/ml) 2 ml/kg | 6 | 10 | 20 | 40 | 60 | 80 | 100 | 100 | ml |
| Defibrillation 4 J/kg | 12 | 20 | 40 | 80 | 120 | 150-200 | 150-200 | 150-360 | J |
| Endotracheal tube inner diameter | 3 | 3.5 | 4 | 5 | 6 | 7 | 7 | 7 | mm |
| *Amiodarone 50 mg/ml. 6 ml diluted with 14 ml glucose 50 mg/ml = 15 mg/ml | |||||||||
For VF/Pulseless VT
- Adrenaline 0.01 mg/kg after the third defibrillation. Repeat every four minutes.
- Amiodarone 5 mg/kg after the third defibrillation. Repeat the same dose after the fifth defibrillation.
Correct Reversible Causes
- Hypoxia
- Hypovolemia
- Hypothermia
- Hyper/hypokalemia
- Hypoglycemia
- Tamponade
- Tension pneumothorax
- Toxic conditions
- Thromboembolism
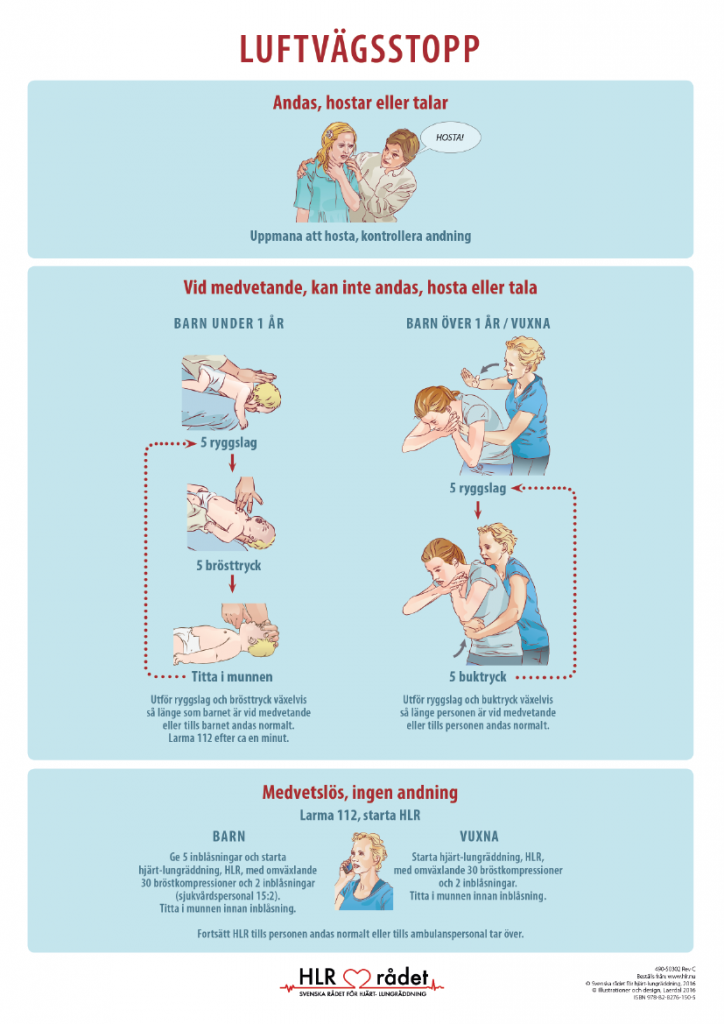
CPR for Children
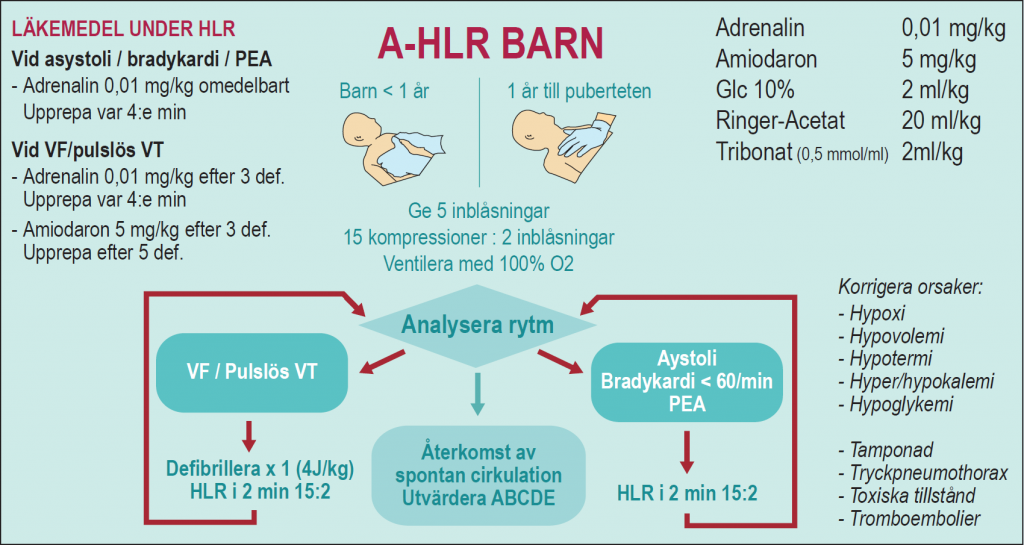
If there are no signs of life in the child: Start CPR with five breaths. Then perform three sets of 15 compressions and two breaths. Call for help. Continue CPR by alternating between 15 compressions and two breaths until help arrives or the child begins to breathe normally.

Cardiopulmonary Resuscitation (CPR)
CPR should be ongoing all the time. Do not pause to check breathing or pulse. If possible, change the person doing the compressions every two minutes. Only stop CPR if the child begins to breathe normally. Remember not to take too long between compressions and breaths.
Check in order: Consciousness. Breathing. Are there signs of life? Isthe child moving, swallowing, or breathing normally? Then provide the necessary help.
- Is the child conscious? Call out to the child and gently pinch or shake their shoulders. If the child does not react, call loudly for help from those around you. Lay the child on their back.
- Is the child breathing? Ensure an open airway. See if the chest and abdomen are moving and check the child’s color. Listen for air flowing in and out through the mouth and nose. Feel the air stream against your cheek. If the child is breathing normally: Place them in the recovery position. Continue to check that the child is breathing. Call for help. If the child is not breathing: Give five slow breaths. If it is not possible to blow or if the chest does not rise during breaths, there may be an object lodged in the child’s throat.

An open airway can be created in two ways: Chin lift. Gently tilt the child’s head back by placing one hand on the child’s forehead. Lift the child’s chin with the index and middle fingers of the other hand. For younger infants, it is important not to tilt the head too far back. Tilting the head back too far can block the airway. Jaw thrust. Place one hand on the child’s forehead. Use the thumb of the other hand to grasp the infant’s lower gum line and the lower gum line of children over one year. Hold the chin with the index finger and lift the chin upward. Breaths. Infants aged 0-1. Perform a chin lift. Place your mouth over the child’s mouth and nose. Blow air slowly for 1-1.5 seconds, five times. Blow in enough air to make the chest rise and fall. Check for signs of life, movement, swallowing, or normal breathing during the breaths.
Infants 0 to 1 Year
The baby can lie on a hard surface. Start with five breaths. Use your index and middle fingers to press on the lower third of the sternum. Press 15 times, nearly two presses per second. Each time, press down on the baby’s chest by one-third. Release the chest between presses (compressions). After 15 presses, give two breaths. Then start again, with 15 presses followed by two breaths. If you are alone, call 112 after three sets of 15 presses and two breaths. Continue with CPR, 15 presses and two breaths, until help arrives or the child breathes normally.
Children 1 Year to Puberty
Pinch the nostrils with your thumb and forefinger. Place your mouth over the child’s mouth and blow air slowly for 1-1.5 seconds, five times. Blow in enough air to make the chest rise and fall. Check for signs of life, movement, swallowing, or normal breathing during the breaths.
- Is the child showing signs of life?
If the child shows signs of life but is not breathing normally: Give 20 breaths per minute and then call 112. If possible, carry the child with you to the phone if you are alone. Continue to give breaths. About 20 breaths per minute is appropriate. If the child shows no signs of life: Start CPR.
A-CPR for Children
Glasgow Coma Scale for Children
Topical Anesthesia for Skin
EMLA (Medical Patch: 25 mg Lidocaine/25 mg Prilocaine)
- 0-3 months: 1 patch for 1 hour, not longer!
- 3-12 months: 1-2 patches for 1 hour
- > 1 year: 1 or more patches (max 10 patches according to operation) for 1-5 hours
Rapydan (70 mg Lidocaine/70 mg Tetracaine)
- Children > 3 years: 1-2 patches (max 2/day) 30 minutes to maximum effect
- Tapin (Cream: Prilocaine 25 mg/g + Lidocaine 25 mg/g)
- Maxilene Cream: Lidocaine 40 mg/g
- Versatis Medical Patch: Lidocaine 700 mg (5%)
Vascular Access
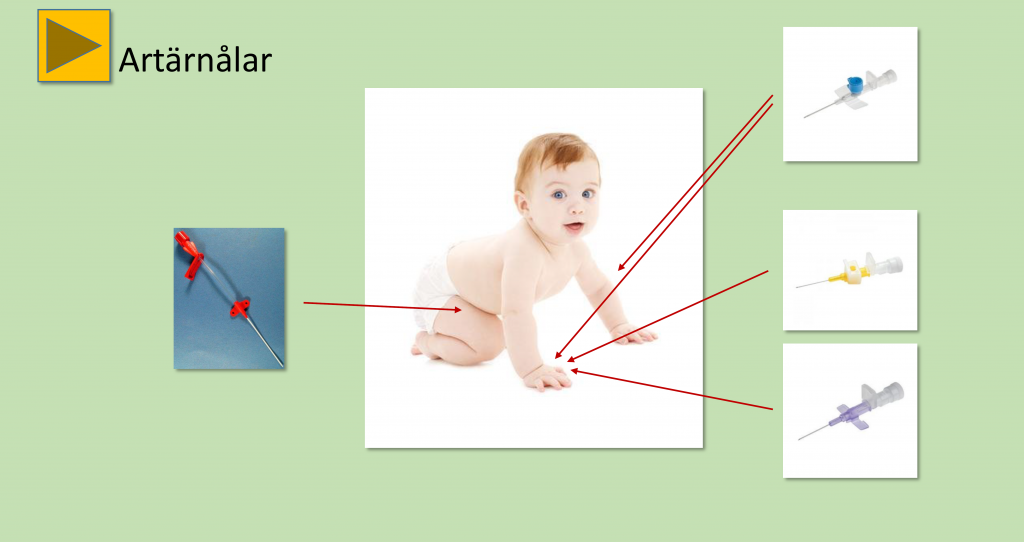
Suggestions for positions and sizes of arterial needles for small children. Note the larger and longer cannula for the femoral artery.
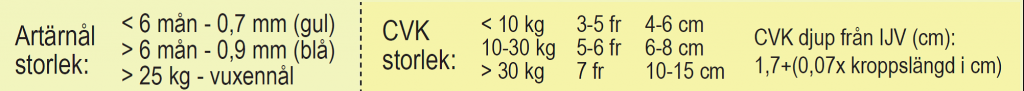
Central Lines
- Do not be afraid to place a central venous catheter (CVC) in anesthetized children! It is trickier in awake patients…
- Check if an echocardiogram has been performed, especially in children with syndromes (systemic venous anatomy).
- Technique is generally the same as for adults in larger children (> 10 kg).
- Choose a vessel you are comfortable with—but for smaller children, the right internal jugular vein is the safest.
- Aim the catheter tip at the right atrium or the transition of the superior vena cava/right atrium.
- Use fluoroscopy if you are unsure.
Central Lines – Smaller Children
- When you get blood return, remove the syringe and release the needle.
- Check that blood still returns from the needle.
- Preferably use a nitinol guidewire (already included in smaller CVC sets made by Arrow) – safer and increases success rates.
- Remove the guidewire from the plastic hoop before you start.
- Rake the end first in smaller children (the bend won’t fit in the vessel).
- Be gentle when advancing the guidewire.
CVL Size (Central Venous Catheter)
- < 10 kg: 3-5 Fr/4-6 cm
- 10-30 kg: 5-6 Fr/6-8 cm
- > 30 kg: 7 Fr/10-15 cm
CVC Depth – IJV right (cm)
- 1.7 + (0.07 x cm height)
Arterial Needles
- Can be placed in the same locations as in adults.
- The brachial artery is a good alternative to the radial artery but may result in poor circulation in the arm.
- The femoral artery is often the best choice if you are in a hurry or want high reliability (may, however, also cause poor circulation – possibly should be avoided in children < 3 kg).
- Heparin is recommended in the flush solution for arterial pressure on PICU (so a-PTT and similar cannot be taken from the artery).
- Ultrasound is often useful for insertion.
Arterial Needle Size
- < 6 months – 0.7 mm (yellow cannula)
- > 6 months – 0.9 mm (blue cannula)
- > 25 kg – adult needle
Intraosseous Needle
- 15 mm < 40 kg
- 25 mm > 40 kg
Nutrition for Children
Fluid and Caloric Needs
- Full-term infant > one week old: 100-150 ml/kg/day (normally for PICU patients, stay on the lower range).
- One-year-old: approximately 100 ml/kg/day.
- 10 years old: approximately 50 ml/kg/day.
- Adjustments should be made based on the current condition. Postoperatively after major surgery, 2-3 ml/kg/h is recommended for the first day.
Normal Energy Requirements at Different Ages
- Premature – neonatal: 110-120 kcal/kg/day
- Full-term newborn – 1 month: 90-100 kcal/kg/day
- 1-7 months: 75-90 kcal/kg/day
- 7-12 months: 60-75 kcal/kg/day
- 12-18 months: 30-60 kcal/kg/day
Enteral Nutrition
- Enteral nutrition can be started immediately unless the surgeon objects.
- For smaller children, give 5 ml x 6 –8, and increase if gastric retention is reasonable.
- Addex-Na and Kajos can be added, preferably when reaching higher food amounts to avoid abdominal discomfort.
- Naloxone APL (10 µg/kg x 4 orally) is given enterally to all receiving opioid infusions (motility agents are generally not used).

Parenteral Nutrition
Initiation of Parenteral Nutrition
- It is somewhat unclear when it is optimal to start parenteral nutrition, likely not suitable in the first days for critically ill children.
- Recommended “if enteral energy intake is expected to be < 50% for > 2-5 days.”
- Three-chamber systems can be used in children > 2.5 kg (e.g., Numeta G16E). Energy content 1 kcal/ml. Not suitable in liver or kidney failure (use separate infusions in these cases).
- Until recently, separate infusions of Clinoleic, Vamin, and glucose were used.
- Larger children (teenagers) can receive Kabiven or similar in the same way as adults.
- All mixtures should be ramped up over three days. Monitor transaminases, bilirubin, and triglycerides in plasma.
Indications for PN
Parenteral nutrition is initiated when the child’s nutritional needs cannot be met with oral and/or enteral nutrition. Where possible, PN should be combined with enteral nutrition. Initiate PN if nutritional intake is less than 50% of the requirement for a period longer than indicated in Table 1 (rule of thumb). The exception is premature infants, where nutritional therapy is initiated immediately after birth.
Maximum period of time with nutritional intake less than 50% of energy needs before PN is started
| The child's age | Day |
|---|---|
| Prematurely born babies | Begins immediately after birth |
| Mature children | Can wait at most |
| < 1 month | 2 days |
| 1 month – 1 year | 3 days |
| > 1 year | 4-5 days |
For losses from the intestine (drain, stoma), pleura (drain), or central nervous system (CSF drainage), these losses should be replaced separately through isotonic infusion fluids and not within the prescribed PN volumes.
Fluid and Nutrition Needs
The child’s energy requirements determine the amount of PN prescribed. PN solutions are energy-dense, and a prescription based on fluid needs results in excessive intake of energy and nutrients. If the patient requires additional fluid, it is prescribed in the form of another infusion solution. Ensure there is no dehydration, acid/base imbalance, electrolyte disturbance, or impact on renal or liver function before starting PN. Dehydration, acid/base, or electrolyte disturbances should be corrected before initiating PN treatment. If the child has significantly impaired renal or liver function, PN may need to be modified (e.g., reduction in protein or fat amounts). This should be discussed with a gastroenterology consultant.
Energy requirements are affected by nutritional status and disease state. In critically ill children with metabolic stress (sepsis, intensive care), energy needs are reduced to about 50-70% of normal. According to the latest research, it is not advantageous to initiate PN treatment within the first days in critically ill children in intensive care 3.
The child's total protein needs
Protein requirement per kg of body weight| Age group | Gram/kg body weight/day |
|---|---|
| Children born before w.37 and during the neonatal period | 1,5 - 4,0 |
| Full-term infants | 1,5 - 3,0 |
| 2 months – 3 years | 1,0 - 2,5 |
| 3-18 years | 1,0 - 2,0 |
Normal energy requirement in children per kg/body weight by age
| Age (years) | Kcal/kg/day |
|---|---|
| Premature - neonatal: | 120-110 kcal/kg/day |
| Full-term newborn - 1 year: | 100-90 kcal/kg/day |
| 1-7 years: | 90-75 kcal/kg/day |
| 7-12 years: | 75-60 kcal/kg/day |
| 12-18 years | 60-30 kcal/kg/day |
Parenteral nutrition for children according to weight and age
The child's total energy needs in ml per kg. The energy content is approximately 1 kCal/ml| Age (years) | Kcal/kg body weight/day | ml/body weight/day |
|---|---|---|
| Full-term newborns-1 | 100-90 | 100-90 |
| 1 to 7 years | 90-75 | 90-75 |
| 7 to 12 years | 75-60 | 75-60 |
| 12 to 18 years | 60-30 | 60-30 |
The child's total fluid needs
Fluid requirements per kg of body weight (Holliday-Segar)| Weight (kg) | Quantity per day |
|---|---|
| Children born before w.37 and during the neonatal period | See PM for patients at Neonatal |
| < 5 kg | 150 ml/kg |
| 5 -10 kg | 100 ml/kg |
| 11 - 20 kg | 1000 ml + 50 ml for every kg over 10 kg |
| > 20 | 1500 ml + 20 ml for every kg over 20 kg |
Vitamins and minerals should be included in full amounts from day 1 when starting PN (for dosage see Table 5). In products ordered from APL, these are already added, but in standardized three-chamber bags, they need to be added. The supplements used in combination are Soluvit, Vitalipid, and Peditrace/Addaven.
Dosage of vitamins and trace elements per day
| Age | Younger than 11 years | Older than 11 years | ||
|---|---|---|---|---|
| Weight | < 10 kg | 10-15 kg | > 15 kg | |
| Soluvit® | 1 ml/kg | 10 ml | 10 ml | 10 ml |
| Vitalipid infant® | 10 ml | 10 ml | 10 ml | |
| Vitalipid adult® | 10 ml | |||
| Peditrace® | 1 ml/kg | 1 ml/kg | ||
| Addaven® | 0,1 ml/kg (max 10 ml) | 0,1 ml/kg (max 10 ml) | ||
Part of a Bag
A patient who is 2 months old and weighs 4 kg is prescribed 400 ml Numeta G16E® (= 412 kCal). The bag size is 500 ml, so only 80% of the bag is given to the patient. To meet the daily requirement of vitamins and minerals, the supplements need to be adjusted.
Multiple Bags
If more than one three-chamber bag is given during the same day, vitamin supplements should be added to the first bag.
Ramping Up PN
Ramping up parenteral nutrition is based on the child’s condition. During the ramp-up, the remaining amount of fluid needed to meet fluid requirements should be given separately. Below is a suggestion for ramping up PN. Day 1 33%, Day 2 67%, Day 3 100%. The prescribed amount should be given over as much of the day as possible; full amounts should not be given in less than 16 hours/day. The recommended infusion time is 20 hours. PPN can be given in a shorter time, but the infusion rate must not exceed the maximum infusion rate according to the product summary, which is 5.5 ml/kg/hour.
Determine the child’s total energy needs, see below. Consider the patient’s condition to determine energy needs. Since the energy content is about 1 kcal/ml, it can easily be converted to volume, see below.
The child's total energy needs
| Age (years) | Kcal/kg body weight/day | ml/kg/day |
|---|---|---|
| 1 - 7 years | 90-75 | 90-75 |
| 7 - 12 years | 75-60 | 75-60 |
| 12 - 18 years | 60-30 | 60-30 |
The development of elevated liver values during PN treatment usually signals ongoing inflammation, steatosis (accumulation of fat in liver cells), and/or impaired bile flow (cholestasis) in the liver. Be particularly vigilant for the development of cholestasis (i.e., conjugated bilirubin > 20 micromol/L), but even mild elevations in other liver values lasting more than a few days are reasons to contact a gastroenterologist for discussion on appropriate management and consideration of the need for investigation of any other underlying causes. If this assessment concludes that the cause of liver impact is PN-related, adjustments to the amount and type of fat in the PN solution may be necessary, often in combination with adjustments in glucose and protein amounts. This type of liver impact seen during relatively short-term use of PN is usually benign and reversible.
The most serious form of liver disease seen during PN treatment is that which affects intestinal failure patients on long-term PN. This condition is called Intestinal Failure Associated Liver Disease, IFALD (previously also known as parenteral nutrition-associated liver disease/cholestasis, PNALD/PNAC) and refers to a progressive liver disease seen in these patients. The diagnosis is clinical, and requires, in addition to intestinal failure and long-term PN, the presence of cholestasis (conjugated bilirubin > 20 micromol/L). The etiology is multifactorial, but the risk of developing IFALD can be reduced, among other things, by using an optimally composed PN solution, especially concerning fat. Modified fat composition (fish oil-based fat emulsion) in PN is also the basis for treating already developed IFALD.
Complications under treatment with TPN
| Complication to TPN | Cause | Proposed action |
|---|---|---|
| Infection in central entrance | Bacterial contamination of entrance | Antibiotic treatment Consider changing the entrance Taurolock® can be used to prevent infections |
| Hyperglycemia | High glucose supply For fast delivery Diabetes | Reduce the feed rate If necessary, give insulin |
| Nausea | For fast delivery Too high energy level Dehydration | Exclude reasons other than PN Lower energy level and speed Provide solution with lower osmolality Ev. antiemetics |
| Tachycardia Fever Rapid weight gain | Refeeding syndrome Fat overload syndrome Kidney failure Infection | Lower energy level and speed Weight control 1 time / day Temp controls Check electrolytes (phosphate, magnesium and potassium drops, in refeeding syndrome) Sepsis investigation, infection tests Coagulation tests in Fat overload syndrome |
| Rising liver values | Cholestasis Liver steatosis Hypertriglyceridemia Chronic inflammation | Change fat emulsion (for example Omegaven®) Stimulate the gut with enteral nutrition Reduce fat content and speed Put possibly. in Ursofalk® Consider antibiotic treatment |
| Rising urea | Impaired renal function Too high nitrogen supply Too low energy supply | Investigation of kidneys / urinary tract Reduce nitrogen supply Increase energy supply |
| Hypertriglyceridemia | Incorrect sampling Too high fat supply Liver failure | Recheck of S-TG Discuss ev. fat reduction with gastroconsultation |
Pain Assessment Scale for Children 0-7 Years

FLACC – Face, Legs, Activity, Cry, Consolability
For pain assessment of children 0-7 years, a behavior scale is used for pain assessment; it can also be used for children with multiple disabilities.
- Observe the child for a few minutes and then look at the categories face/legs/activity/cry/consolability to see if the score is 0, 1, or 2 that fits the child.
- Then sum the points, with a maximum of 10 points.
- A value of < 3 is aimed for. At values < 4, a nursing intervention may be sufficient, at values > 4, pain relief should be considered.
- Whenever pain is suspected and nursing interventions do not help the child, a trial with analgesics should be conducted. Evaluate the result with pain assessment.
FLACC Behavioral Scale Children
| Try to observe the child for at least 2 minutes | 0 points | 1 points | 2 points |
|---|---|---|---|
| Face | Neutral facial expressions or smiles | Bister eyesight, wrinkles the forehead occasionally, withdrawn, uninterested | Frequent or constantly wrinkled brow, trembling chin, bumpy jaws |
| Legs | Normal position or relaxed | Worried, restless or tense legs | Kicking or legs drawn |
| Activity | Stands calm, normal position, moves unobstructed | Screws, often changes position, tense | Arc, raises or stems |
| Crying | No crying (awake or sleeping) | Gnaws or smells, complains off and on | Crying persistently, screaming or sneaking, complaining often |
| Ability to comfort | Satisfied, relaxed | Can be calm with touch, hugs or chatting. Distractable. | Hard to comfort or calm |
AS Face Scale
AS is a modified VAS scale for children aged 5-18 years. It consists of six faces, with the 1st face counted as 0 points and the 6th face as 10 points. At 4 points and above, pain relief should be considered. Note that some children may confuse emotional states with pain. Do not ask “Does it hurt?” instead ask “Do you feel anything from the wound?” If the answer is yes, ask, “How does it feel?” If the child acknowledges pain, ask, “How much does it hurt?” “Can you show me on the scale?”.

The face scale is analogous to The Faces Pain Scale (FPS; Bieri et al., Pain 41 (1990) 139).
Syringe Sizes for Medications for Children
Recomended Syringe Sizes for Children up to 15 kg
| Medication | Syringe size |
|---|---|
| Propofol | 5 ml syringe |
| Ketamine | 5 ml syringe |
| All muscle relaxants | 1 ml syringe |
| Fentanyl | 1 ml syringe |
| Morphine | 1 ml syringe |
| Alfentanil | 1 ml syringe |
| Anticolinergics (Atropine, Glycopyrrolone) | 1 ml syringe |
| Glycopyrrolone (Robinul-Neostigmine®) | 1 ml syringe |
| Sodium Thiopentone (Pentothal®) | 5 ml syringe (sodium thiopentone) |
Recomended Syringe Sizes for Children over 15 kg
| Medication | Syringe Size |
|---|---|
| Propofol | 10 ml syringe |
| Ketamin | 10 ml syringe |
| All muscle relaxants | 3 ml syringe |
| Fentanyl | 3 ml syringe |
| Morphine | 3 ml syringe |
| Alfentanil | 3 ml syringe |
| Anticolinergics (Atropine, Glycopyrrolone) | 1 ml syringe |
| Glycopyrrolone Robinul-Neostigmine® | 1 ml syringe |
| Sodium Chloride | 10 ml alternatively 5 ml syringe |
| Succamethonium | Branded with white syringe label with red text. |
| Sodium Thiopentone (Pentothal®) | 10 ml syringe (thiopentalnatrium) |
Thromboprophylaxis in Immobilization
- No immobilization prophylaxis in children before puberty.
- After that, Fragmin approximately 100 IU/kg x 1 up to normal adult doses.
- When treating an existing thrombosis, higher doses are often required, especially in small children. Monitor anti-Xa (should be 0.5 –1.0).
- We also check antithrombin and keep the value > 0.7 during all heparin treatment.
Urine Production in Children

Urine Production in Children per Hour
- 0-2 years: 1.5-2 ml/kg/h
- 3-5 years: 1-1.5 ml/kg/h
- 6-12 years: 0.5-1 ml/kg/h
Bladder Capacity
- Children < 12 years = age x 30 ml + 30 ml
- Children > 12 years: 350-500 ml
Catheter Size (Foley Catheter)
- < 1 year: 6 Fr
- 1-6 years: 8 Fr
- 8-12 years: 10-12 Fr
- 13-16 years: 10-14 Fr
Antiemetics for Children
PONV Risk
- > 3 years of age
- Long anesthesia time
- Eye/ENT surgery
- Motion sickness
- Previous PONV
Prophylaxis
- Propofol induction
- Evacuate air from the stomach
- Keep the patient well-oxygenated
Treatment
- Ondansetron iv 0.1 mg/kg (max 4 mg)
- Betapred iv 0.2 mg/kg (max 4 mg)
- Dridol (not for children < 2 years) iv 0.02 mg/kg (max 1.25 mg)
Ondansetron to Children Dose mg/kg
| Weight (kg) | Intravenous Dose Solution 2 mg/ml | Weight (kg) | Oral dose Solution 0,8 mg/ml | Oral dose Tablet |
|---|---|---|---|---|
| ≥1 months: 0,1 mg/kg | Max 4 mg x 4 | ≥1 months: 0,2 mg/kg | Max 8 mg x 4 | |
| 8 - 14 kg | 1 mg = 0,5 ml | < 15 kg | 2 mg = 2,5 ml | 2 mg |
| 15 - 24 kg | 2 mg = 1 ml | 15 - 30 kg | 4 mg = 5 ml | 4 mg |
| 25 - 34 kg | 3 mg = 1,5 ml | > 30 kg | 8 mg = 10 ml | 8 mg |
| > 35 kg | 4 mg = 2 ml |
Other Antiemetics for Children
| Drug | Route | Remarks |
|---|---|---|
| Betametasone 4 mg/ml | Intravenous injection | |
| Dosage | 2 mg/kg | Max dose 4 mg x 1 |
| Metoclopramide 5 mg/ml | Intravenous injection | Children ≥ 1 year |
| Dosage | 0,15 mg/kg/dose | Max dose 10 mg x 3 |
| Phenergan 25 mg/ml | Children ≥ 1 year | |
| Intravenously | 0,5 mg/kg | |
| Orally | Tablet or Solution | Children ≥ 1 year. Max dose 25 mg x 4 |
| Droperidol 2,5 mg/ml | Intravenously 0,010 - 0,075 mg/kg | Max dose 1,25 mg x 4-6 |
Premedication with Intranasal Sufentanil for Children
Indication
Children who are to receive anesthesia where sedation is deemed appropriate before induction.
Contraindication
Ongoing nasal bleeding or other nasal obstruction.
Administration of sufentanil intranasally requires the presence of anesthesia personnel, the ability for continuous monitoring, and possible ventilation support.
Effect
Sedation is usually achieved within 10-15 minutes, and maximum analgesic effect occurs after 20-25 minutes. In some patients, the effect can occur within a few minutes.
Dosage/Administration
- Sufentanil 1 microgram/kg (50 micrograms/ml) is given with a 2 ml syringe connected to a Mucosal Aerosol Device (MAD). Use a Luer Lock syringe to prevent the MAD from detaching during injection.
- Total dose 1-2 micrograms/kg: Half the dose is administered in each nostril.
- Administer 0.1-0.2 ml at a time. When applying, aim upwards inside the nostril in the direction of the eyes (cranial direction).
- Apply in both nostrils as quickly as possible. It is important to apply pressure to the plunger to achieve aerosol.
- Uncertain effect at larger volumes, as some of the dose passes beyond the nasal mucosa and is swallowed.
Dosage Table
Sufentanil administered nasally for children
| Weight (kilo) | Dose (microgram) | Volume (ml) |
|---|---|---|
| 10 | 20 | 0.4 |
| 13 | 26 | 0.5 |
| 15 | 30 | 0.6 |
| 18 | 36 | 0.7 |
| 20 | 40 | 0.8 |
| 23 | 46 | 0.9 |
| 25 | 50 | 1 |
| 28 | 56 | 1.1 |
| 30 | 60 | 1.2 |
| 35 | 70 | 1.4 |
| 40 | 80 | 1.6 |
| 45 | 90 | 1.8 |
| 50 | 100 | 2 |
| 55 | 110 | 2.2 |
| 60 | 120 | 2.4 |
References
- Bayrak F, Gunday I, Memis D, Turan A. A comparison of oral midazolam, oral tramadol, and intranasal sufentanil premedication in pediatric patients. J Opioid Manag. 2007 Mar-Apr;3(2):74-8.
- Zedie N, Amory DW, Wagner BK, O’Hara DA. Comparison of intranasal midazolam
Acute Poisoning in Children
Children who have been poisoned by medications, chemicals, or other household products should primarily be transported to a pediatric clinic, but if the condition is life-threatening, they must be transported to the nearest emergency hospital for primary care. In cases of carbon monoxide poisoning leading to unconsciousness, the child should, if possible, be taken directly to a clinic capable of providing hyperbaric oxygen therapy in a pressure chamber.
The most common poisonings in children are caused by household products, chemicals, and cleaning agents. Severe poisonings occur after ingestion of medications such as calcium channel blockers, beta-blockers, antidepressants, and digitalis. Poisoning with heavy metals and various mushrooms also occurs and is often associated with intense vomiting and diarrhea.

Once the child’s vital signs have been assessed, ensure an open airway. The child receives oxygen and is placed in the recovery position if drowsy or unconscious. They may also receive a peripheral venous cannula and fluids (Ringer’s acetate, sodium chloride). In cases of opioid poisoning, antidote treatment with naloxone is administered (the recommended initial dose is 0.01–0.02 mg/kg), and in benzodiazepine poisoning, flumazenil is given (at the recommended starting dose of 0.01 mg/kg up to 0.2 mg).
Dosing of emetic syrup for children
| The child's age | < 1 year | 1–5 years | > 5 years |
|---|---|---|---|
| Dose | 5–10 ml | 7,5–15 ml | 15–30 ml |
Activated charcoal should be administered in cases of life-threatening overdoses or poisonings with substances that adsorb to charcoal when a pronounced toxic reaction is feared. Nearly all medications bind to activated charcoal except for iron and lithium, and potassium adsorbs poorly to charcoal as well. Ethanol, methanol, and cyanides also do not bind to activated charcoal. Activated charcoal suspended in water can also be given pre-hospitally if the patient is cooperative. However, it should not be given if there is a significant risk of vomiting and lung aspiration of charcoal.
The administration of activated charcoal without gastric lavage can be applied when the poisoning is considered mild to moderate (unaffected vital signs) or when the patient arrives relatively late after the poisoning incident, e.g., more than an hour after drug intake or in the late stage of mushroom poisoning.
Children up to one year of age should be given 1 g/kg body weight. Children between 1 and 12 years of age should be given 25-50 g. Adolescents and adults should be given 25-100 g of charcoal in a single dose.
Dosage of diluted medicinal charcoal for children
| Age | Dose |
|---|---|
| < 1 year | 50–100 ml |
| 1–3 years | 100 ml |
| 3–5 years | 100–250 ml |
| > 5 years and adults | 250 ml |
In certain severe poisonings, the administration of activated charcoal should be repeated four to six times during the first 24 hours. This procedure is simply called “Repeated Activated Charcoal.”
Disclaimer:
The content on AnesthGuide.com is intended for use by medical professionals and is based on practices and guidelines within the Swedish healthcare context.
While all articles are reviewed by experienced professionals, the information provided may not be error-free or universally applicable.
Users are advised to always apply their professional judgment and consult relevant local guidelines.
By using this site, you agree to our Terms of Use.