Author:
Kai Knudsen
Updated:
26 November, 2025
Here, a range of nerve blocks with local anesthetics for surgical anesthesia are described. Techniques using ultrasound, videos and images of anatomical landmarks and underlying structures are included. Appropriate choices of local anesthetics with suggested dosages are also discussed.
- Adductor Canal Block/Subsartorius Block
- Axillary Plexus Block
- Caudal Block
- Dosage of local anesthetics in common blocks
- Fascia Iliaca Compartment Block (FICB)
- Femoral Block
- Foot Block
- Intravenous Regional Anesthesia (IVRA)
- Ilioinguinal Block
- Infiltration Anesthesia
- Infraclavicular Plexus Block
- Interscalene Block
- Local Anesthetic Systemic Toxicity (LAST)
- Intravenous Lipid Emulsion Therapy
- Nerve Block on Fingers and Toes
- Paravertebral Block
- PECS I and II Block
- Continuous Peripheral Nerve Block (PNB) – Checks
- Popliteal Block
- Rectus Block (Rectus Sheath Block, Paraumbilical Block)
- Saphenous Block
- Sciatic Nerve Block
- Serratus Plane Block
- Supraclavicular Plexus Block
- Suprazygomatic Maxillary Block
- TAP Block (Transversus Abdominis Plane)
- Thoracic Epidural Block (Ultrasound-Guided)
- Regional Anesthesia Pocket Guide
Adductor Canal Block/Subsartorius Block
Indication: Blockade of the saphenus nerve – nervus saphenus . Surgery involving saphenous vein stripping. Adjuvant in medial foot/ankle surgery combined with sciatic nerve block and analgesia for knee surgery combined with other pain relief. Provides anesthesia on the medial side of the leg.
Technique: Transverse anteromedially on the thigh at the junction between the middle and distal third of the thigh or below the knee at the level of the tibial tuberosity.
Body Position: Flat supine position
Transducer: 10-16 MHz, linear probe (“Hammerhead”)
Probe Position: In-plane technique (along the probe held transversely over the leg), lateral insertion.
Injection Needle: 22G, 8 cm long, bevel tip.
Set Depth in Ultrasound Image: 2.5-4 cm.
Ideal Image: Blockade of saphenus nerve. The local anesthetic spreads laterally in the thigh and deep toward the sartorius muscle or more distally below the knee, adjacent to the saphenous vein.
Note the Anatomy: The saphenous nerve is a terminal sensory branch of the femoral nerve. It supplies innervation to the medial side of the leg down to the ankle and foot. The nerve also sends infrapatellar branches to the knee joint. A blockade of saphenus nerve is useful as an adjunct to ischiadicus block for foot and ankle procedures involving the medial malleolus and foot.
Selection of local anesthetic agent for Adductor Canal Block
| Local anesthetic agent | Volume (ml) | Onset time | Duration |
|---|---|---|---|
| Ropivacaine 5 mg/ml | 20-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 7,5 mg/ml | 15-20 ml | 10-45 min | 3-9 hours |
| Mepivacaine 10 mg/ml | 30 ml | 10-20 min | 2-5 hours |
| Lidocaine 10 mg/ml | 30 ml | 10-20 min | 1-4 hours |
Axillary Plexus Block
Indication: Anesthesia for surgery of the elbow, forearm, or hand.
Body Position: Supine position with the arm bent at the elbow and hand raised above the head. Slight head-down tilt on the bed, pillow under the arm. The anesthesiologist can sit either below or above the patient’s arm. Preferably, an assistant can perform the injection of the local anesthetic as three hands are practically needed for this block.
Technique: Preferably use the in-plane technique with needle insertion from the lateral side of the ultrasound probe. Insert the needle under the probe parallel to the probe head. The target for the needle tip is inside the plexus sheath. Perform as few injections as possible, preferably 2-3, deep and lateral to the artery. Ideal spread is around the hyperechoic nerve root structures, about 5 ml at each site. Observe hydrodissection, i.e., the filling of the plexus sheath with anesthetic fluid (LA). During correct hydrodissection, a temporary compression of the artery often occurs. The injection needle is much more visible in the image with the in-plane technique than with the out-of-plane technique.
Out-of-plane (visualisation across the brachial artery): Provides the image of the axillary artery as a pulsing hypoechoic sphere. The needle is inserted along the probe head from the lateral side cranially to the probe head. The needle tip is placed posterior (below) and lateral to the artery.
With the out-of-plane technique, the needle is inserted at the level of the probe head’s midpoint, centrally under the probe’s midpoint. The needle should come down into the image vertically in the midline. The needle or needle movements can still be visualized in the image. Jiggle the needle regularly to see it in the image. If difficulty visualizing the brachial vein occurs, it is often due to excessive probe pressure against the axilla. Lighten the pressure and the vein can usually be visualized. The vein normally lies just medial to the artery.
In-plane (along the brachial artery): Provides a longitudinal section of the artery, allowing deposition of local anesthetic with clear hydrodissection of the nerve sheath that lifts during the injection process. Clearly reveals incorrect injection.
Transducer: 10-16 MHz, linear probe (“Hammerhead”).
Probe Position: Either out-of-plane technique (transverse) or in-plane technique (transverse or longitudinal) with the axillary artery in the axilla. Primarily in transverse just distal to the midpoint of the axilla.
Injection Needle: 22G, 5 cm long, bevel tip.
Nerve Stimulation Response: Hand.
Set Depth in Ultrasound Image: 2.5-3 cm.
Ideal Image: Out-of-plane (transverse): Provides the image of the axillary artery as a pulsing hypoechoic dark sphere. The technique aims to block median nerve, ulnar nerve, radial nerve, plus n. musculocutaneus. The nerves are usually hyperechoic slightly smaller spherical structures. Observe hydrodissection during the injection phase.
Note the Anatomy: The artery lies within the nerve-vessel sheath that can sometimes be identified with ultrasound. Three nerve structures can be identified around the artery as hyperechoic zones, usually median nerve at 12-13 o’clock, ulnar nerve at 16-17 o’clock, and radial nerve at 18-19 o’clock if the artery is compared to a clock face. Anatomical variations occur.
N. musculocutaneus (McN) lies laterally a bit out and below the axillary artery, outside the nerve-vessel sheath. To reach the n. musculocutaneus, a slightly longer needle is usually needed, 8 cm. The appearance of McN is more elongated and triangular compared to the other nerves in the axilla, blocked with only 3-5 ml LA.
Selection of local anesthetic agents for Axillary Plexus Block
| Local anesthetic agent | Volume (ml) | Onset time | Duration |
|---|---|---|---|
| Mepivacaine 10 mg/ml | 20-40 ml | 10-20 min | 2-5 hours |
| Ropivacaine 5 mg/ml | 10-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 7,5 mg/ml | 15-20 ml | 10-45 min | 3-9 hours |
| Lidocaine 10 mg/ml | 20-40 ml | 10-20 min | 1-4 hours |
Warning: Avoid puncturing the brachial artery or brachial vein. Do not inject into the nerves themselves, observe and avoid heavy injection resistance. In case of accidental arterial puncture, withdraw the needle and compress firmly for 3-5 minutes. Then repeat the needle insertion with better visualization using the in-plane technique.
Caudal Block
Indication: Anesthesia for surgery of the urogenital tract of small children or caudal postoperative pain relief.
Caudal block is mainly used as an alternative to epidural anesthesia in small children for postoperative analgesia after surgery on the lower half of the body. The sacral block is administered by placing a needle through the sacral hiatus to deliver local anesthetic into the epidural space. This technique is used not only for surgical anesthesia and pain relief in children but also for managing various chronic pain conditions in adults. The caudal block can be advantageously administered after waking up in connection with anesthesia for surgery.
The patient can be placed in a prone or lateral position for a caudal blind technique. A line is drawn to connect the upper bilateral iliac crests, used as one side of an equilateral triangle; then, the sacral location is approximated. By palpating the sacral Cornua as two bony protrusions, the sacral hiatus can be identified as a groove in the center. An epidural needle is inserted at 45 degrees to the sacrum and redirected if contact is made with the posterior surface of the sacrum. A subjective sensation of “loss” or loss of resistance occurs upon penetration but is associated with a failure rate of up to 26% even in experienced hands.
Caudal block for surgical anesthesia
| Local anesthetic agent | Concentration | Dose in ml | Dose in mg | Brand name |
|---|---|---|---|---|
| Lidocaine | 10 mg/ml | 20–40 ml | 200–400 mg | Xylocaine |
| Mepivacaine | 10 mg/ml | 15–20–30 ml | 150–200–300 mg | Carbocaine |
| Mepivacaine | 20 mg/ml | Up to 17.5 ml | 350 mg | Carbocaine |
Caudal block on toddlers (< 10 kg) | ||||
| Bupivacaine | 2,5 mg/ml with adrenaline | 0,5 ml/kg | Marcaine | |
| Ropivacaine | 2 mg/ml | 1 ml/kg | Naropin | |
Dosage of local anesthetics in common blocks
Major block
Axillary Plexus Block, TAP Block, Fascia Iliaca Compartment Block (FICB)| Local anesthetic agent | Concentration | Volume (ml) | Onset Time | Duration | Dose (mg) | Drug |
|---|---|---|---|---|---|---|
| Lidocaine | 10 mg/ml | 10-40 ml | 10-20 min | 1-4 hours | 100-400 mg | Xylocaine |
| Mepivacaine | 10 mg/ml | 20–40 ml | 10-20 min | 2-5 hours | 200–400 mg | Carbocaine |
| Mepivacaine | 20 mg/ml | 10–17,5 ml | 10-20 min | 2-5 hours | 200–350 mg | Carbocaine |
| Ropivacaine | 5 mg/ml | 10-40 ml | 10-45 min | 3-9 hours | 75-300 mg | Naropin |
Small to medium block
Supraclavicular plexus block, Infraclavicular plexus block, Interscalenius block, Femoral block, Ischiadic block, Saphenous block, Ileoinguinal block, Popliteal block, PECS, Serratus Anterior Plane Block, Foot block, Quadratus Lumborum block| Local anesthetic agent | Concentration | Volume (ml) | Onset Time | Duration | Dose (mg) | Drug |
|---|---|---|---|---|---|---|
| Lidocaine | 10 mg/ml | 10-20 ml | 10-20 min | 1-4 hours | 100-200 mg | Xylocaine |
| Ropivacaine | 5 mg/ml | 1-30 ml | 10-45 min | 3-9 hours | 5-150 mg | Naropin |
| Ropivacaine | 7,5 mg/ml | 1-30 ml | 10-45 min | 3-9 hours | 7,5-225 mg | Naropin |
| Mepivacaine | 10 mg/ml | 10–20 ml | 10-20 min | 2-5 hours | 100–200 mg | Carbocaine |
Fascia Iliaca Compartment Block (FICB)
Indications: Anterior thigh and knee surgery, analgesia after hip and knee surgeries.
Fascia iliaca block is an alternative to blocking the femoral nerve or lumbar plexus to anesthetize the lower extremity. This block is feasible because the femoral and lateral femoral cutaneous nerves lie under the fascia iliaca. Therefore, sufficient local anesthetic deposited under the fascia iliaca, even if it is far from the nerves, can spread under the fascia and block these nerves.
Transducer Position: Transverse, near the femur and lateral on the thigh.
Goal: Medial-lateral spread of local anesthetic under the fascia iliaca.
Selection of local anesthetic agents for Fascia Iliaca Compartment Block FICB
| Local anesthetic agent | Volume (ml) | Onset time | Duration |
|---|---|---|---|
| Mepivacaine 10 mg/ml | 20-30 ml | 10-20 min | 2-5 hours |
| Ropivacaine 2 mg/ml | 30-40 ml | 10-45 min | 3-9 hours |
| Ropivacaine 5 mg/ml | 20-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 7,5 mg/ml | 15-20 ml | 10-45 min | 3-9 hours |
| Lidocaine 10 mg/ml | 20-30 ml | 10-20 min | 1-4 hours |
Femoral Block
Indication: Surgery or pain condition on the femur, anterior groin, knee. Anesthesia of the femoral nerve – femoral nerve.
Body Position: Flat supine position.
Technique: Use the in-plane technique with needle insertion on the lateral side of the ultrasound probe’s head. Insert the needle under the probe parallel to the probe’s longitudinal axis in a medial direction above the iliac muscle. The target for the needle tip is lateral and under the femoral nerve. Perform as few injections as possible, preferably 1-2. Ideal spread is around the hyperechoic nerve root structure. Note hydrodissection, i.e., filling around the nerve with LA.
Transducer: 8-16 MHz linear probe (“Hammerhead”).
Probe Position: In the groin just below the inguinal ligament. Place the probe parallel to the inguinal ligament. First, identify the femoral artery, then the femoral nerve. Tape up excess abdominal folds.
Injection Needle: 21G, 10 cm long, bevel tip.
Nerve Stimulation Response: Quadriceps muscle.
Set Depth in Ultrasound Image: 4 cm.
Ideal Image: Visualize the iliac muscle, femoral artery, fascia
iliaca, fascia lata, and femoral nerve.
Note the Anatomy: The femoral nerve lies lateral to the femoral artery with a hyperechoic structure. Note that the nerve lies under the fascia iliaca.
Selection of local anesthetic agents for Femoral Block
| Local anesthetic agent | Volume (ml) | Onset time | Duration |
|---|---|---|---|
| Mepivacaine 10 mg/ml | 15-20 ml | 10-20 min | 2-5 hours |
| Ropivacaine 5 mg/ml | 10-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 7,5 mg/ml | 10-20 ml | 10-45 min | 3-9 hours |
| Lidocaine 10 mg/ml | 20-30 ml | 10-20 min | 1-4 hours |
Warning: Avoid puncturing the femoral artery. If the patient is obese, it may be better with a pillow under the same side’s hip to extend the hip joint if possible.
Foot Block
Indication: Hallux valgus, forefoot surgery. Anesthesia of tibial nerve posterior, deep peroneal nerve, superficial peroneal nerve, and sural nerve.
Patient Position: Flat supine position. The leg is flexed 70 degrees at the knee, angled outward or inward as needed. The block can be performed with or without ultrasound, usually without.
Transducer: 8-16 MHz, linear probe.
Probe Position: The probe is placed transversely over the ankle (a. dorsalis pedis) and medially over the malleolus above a. tibialis posterior.
Injection Needle: 20-22 G, 5 cm long, bevel tip.
Set Depth in Ultrasound Image: 2-4 cm.
Technique: Foot Block consists of three parts.
A) Block of deep peroneal nerve with insertion medially in the middle above the ankle. Move the needle between the extensor hallucis longus tendon and extensor digitorum longus tendon, fan-shaped at about 2 cm depth, aspirate blood and deposit about 5 ml of local anesthetic deep against the extensor retinaculum. This will block deep peroneal nerve. You can also anesthetize slightly lower on the dorsum of the foot by injecting immediately medial to a. dorsalis pedis (see image below).
Withdraw the needle, direct it superficially towards the lateral malleolus. Deposit 3-5 ml subcutaneously to block the superficial deep peroneal nerve. Then direct the needle superficially towards the medial malleolus. Deposit 3-5 ml subcutaneously to block the saphenous nerve.
B) Insert immediately lateral (behind) a. tibialis posterior just behind and below the medial malleolus to anesthetize tibial nerve posterior. Insert the needle posterolaterally to the artery, at the level of the medial malleolus. Advance the needle slowly and carefully, being aware of any paresthesias. Inject 5-8 ml of local anesthetic at about 1 cm depth.
C) A curtain 5-15 cm above the lateral malleolus to anesthetize superficial peroneal nerve laterally to the tibia. Inject 5-10 ml of local anesthetic at about 2 cm depth in a curtain-like fashion. Superficial peroneal nerve innervates most of the dorsum of the foot including the big toe. Below the lateral malleolus, sural nerve is anesthetized, which innervates the lateral side of the foot.
Technique: Use the In plane technique with insertion 0.5 cm from the medial side of the ultrasound probe’s head. Insert the needle under the probe medially to the target. The target for the needle tip is tibial nerve posterior, deep peroneal nerve, superficial peroneal nerve, and sural nerve.
Selection of local anesthetic agents for Femoral Block
| Local anesthetic agent | Volume (ml) | Onset time | Duration |
|---|---|---|---|
| Mepivacaine 10 mg/ml | 15-20 ml | 10-20 min | 2-5 hours |
| Ropivacaine 5 mg/ml | 10-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 7,5 mg/ml | 10-20 ml | 10-45 min | 3-9 hours |
| Lidocaine 10 mg/ml | 20-30 ml | 10-20 min | 1-4 hours |
Warning: Check for any neurological damage, diseases, or symptoms in the patient before administering the block. If paresthesias occur, withdraw the needle by half a centimeter before administering the anesthetic.
Video Link: https://youtu.be/pTKBGTwVuOs
Intravenous Regional Anesthesia (IVRA)
Suitable for relatively short procedures on the hand and foot, primarily the hand. The estimated maximum block time with IVRA is 1.5 hours. Suitable for procedures up to 1 hour of operation time.
Indications
- Surgical procedures up to the elbow region/knee region.
- Closed/open reductions
- Rheumatoid arthritis
- Minor tendon & nerve injuries
- Dupuytren’s contracture
- Ganglion
- Tenolysis
Contraindications
- AV block.
- Allergy to local anesthetics.
- Epilepsy that is not optimally treated.
- Estimated operation time > 1 hour.
- Patient with sickle cell anemia.
- Severe Raynaud’s disease.
- Other circulatory impairment of the arm.
- Infections in the arm/leg.
- Hypertension > 180 mmHg systolic.
Connecting and Monitoring the Patient
- Connect the patient to ECG and saturation.
- Attach the blood pressure cuff on the arm that is not to be operated on and take baseline values.
- Connect oxygen as needed.
- Insert two IV lines, one in the arm that is not to be operated on, and one as distally as possible in the arm/leg to be operated on.
- Connect 1000 ml Ringer’s acetate/Glucose to the arm that is not to be operated on.
- Turn on the tourniquet machine, automatic function check is performed.
- Tubular stockinette under the cuff (see instructions on the device for the bloodless field). Ensure that the stockinette extends well beyond the cuff both above and below.
- Apply the IVRA cuff (with two fields) tightly for a bloodless field. Connect the cuff and machine. Red to proximal = upper, blue to distal = lower cuff channel.
- Never adjust the cuff when applied to the extremity by twisting. Instead, remove it and reapply it. Wrinkle-free application reduces the risk of mechanical injury to the skin.
- Contact the operator and ensure it is okay to administer the anesthesia.
- Elevate the patient’s arm/leg, the one to be operated on, for about 5 minutes (sometimes this may be sufficient before inflating the cuff) or wrap the patient’s arm/leg with Esmarch’s elastic bandage tightly from the fingers/toes all the way to the cuff.
- Inflate the distal lower cuff = blue part of the cuff to about 75-125 mmHg above systolic baseline blood pressure (see below) to empty this part of the blood as well and test that the cuff works.
- Then inflate the upper proximal cuff = red part of the cuff to about 75-125 mmHg above the patient’s systolic baseline pressure and remove the elastic bandage. Ensure the cuff maintains the pressure.
- Now release the pressure in the distal lower blue cuff.
- NOTE: Patients with large forearms/legs or high blood pressure may be insufficient for IVRA, and other methods should be considered.
Cuff Pressure Applied Over the Patient’s Systolic Baseline Pressure:
- For arm 75 – 125 mmHg above.
- For legs 100-150 mmHg above.
- Inject local anesthetic as described below into the IV line in the arm/leg to be operated on after confirming a bloodless field (check pulse, color).
- Remove the IV line from the operative area after the injection.
- The patient often experiences a strong sensation of warmth locally when the anesthesia begins to take effect.
Local Anesthetic Dosage
- Mepivacaine 0.5%: 3 mg/kg = 0.6 ml/kg body weight intravenously, in the venous cannula on the dorsal side of the hand.
- Prilocaine 5 mg/ml ≤ 3 mg/kg body weight ≤ 0.6 ml/kg
- For the arm 20-40 ml 4 mg/kg body weight ≤ 0.8 ml/kg
- For the leg 60-80 ml
- The maximum dose of Prilocaine is 400 mg.
- Minimum dose: 35 ml.
- Maximum dose: 65 ml dose Carbocaine 0.5%: 3 mg/kg = 0.6 ml/kg body weight intravenously, in the venous cannula on the dorsal side of the hand.
- Minimum dose: 35 ml.
- Maximum dose: 65 ml.
Intravenous regional anesthesia (IVRA), Bier's block
| Target Organ | Local anesthetic agent | Volume (ml) | Dose (mg) | Local anesthetic Brand name |
|---|---|---|---|---|
| Mepivacaine 5 mg/ml | 0,6 ml/kg | 3 mg/kg | Carbocain 0,5% | |
| Arm (Hand) | Mepivacaine 5 mg/ml | 20-60 ml | 100-300 mg | Carbocain 0,5% |
| Arm (Hand) | Lidocaine 5 mg/ml | 20–40 ml | 100–200 mg | Xylocain 0,5% |
| Leg (Foot) | Lidocaine 5 mg/ml | 40 ml | 200 mg | Xylocain 0,5% |
| Arm (Hand) | Prilocaine 5 mg/ml | 20-40 ml | 100-200 mg | Citanest 0,5% |
| Leg (Foot) | Prilocaine 5 mg/ml | 60-80 ml | 300-400 mg | Citanest 0,5% |
| Note: Dose of local anesthetic is given intravenously, in a venous cannula on the dorsal side of the hand with a tornique. Minimum dose: 35 ml. Maximum dose: 65 ml. | ||||
Miscellaneous
- Timing:
- Surgery should commence 10-20 minutes after the anesthesia is applied, allowing time for sterilization and preparation.
- Tourniquet Precautions:
- Ensure no alcohol solution seeps under the cuff during sterilization to prevent burns. Both the sock and cuff must remain dry.
- Managing Tourniquet Pressure:
- After 30 minutes, if the patient experiences discomfort from the cuff pressure, you can switch the pressure to the lower distal (blue) cuff after a minimum of 15 minutes, then release the upper proximal (red) cuff.
- Duration of Pressure:
- Do not release the cuff pressure before 20-30 minutes to avoid systemic effects of the local anesthetic and the risk of toxic side effects if pressure is released too soon.
- Monitoring Time:
- Inform the surgeon at 60 minutes, 90 minutes, 105 minutes, 120 minutes, and so on. It is the surgeon’s responsibility to decide how long the pressure should be maintained.
- Post-Pressure Release:
- Once the pressure is released, anesthesia will wear off within 10-20 minutes. The patient may experience a tingling or prickling sensation that usually resolves quickly.
- Post-Operative Pain Management:
- Plan for alternative post-operative pain relief as needed.
These guidelines are crucial for ensuring patient safety and comfort during and after procedures involving anesthesia and a tourniquet.
Ilioinguinal Block
Indication: Femoral neck fracture, inguinal hernia. Anesthesia of n. ilioinguinalis and n. iliohypogastricus.
Patient Position: Flat supine position. Arms outstretched (abducted).
Technique: Use the In plane technique with insertion 0.5 cm from the medial side of the ultrasound probe’s head. Insert the needle under the probe medially to the target. The target for the needle tip is between the internal oblique muscle and the transversus abdominis muscle. Penetration of the posterior fascia can be felt as a “pop” or “release.” Perform as few injections as possible, preferably only one. Note proper hydrodissection, i.e., filling the space between the muscle layers.
Transducer: 8-16 MHz, linear probe.
Probe Position: Just above the iliac crest angled towards the navel. The probe is placed transversely parallel to the rib cage.
Injection Needle: 22 G, 10 cm long, bevel tip.
Set Depth in Ultrasound Image: 3 cm.
Ideal Image: Visualize the iliac crest laterally in the image (spina iliaca anterior superior). The ilioinguinal nerve lies between the transversus abdominis muscle (above) and the internal oblique muscle. The rectus muscle lies medially and is passed out and away.
Note the Anatomy: The transversus abdominis muscle lies under the internal oblique muscle, which in turn lies under the external oblique muscle. Above the external oblique muscle, there is abdominal fat. The nerves lie between the internal oblique muscle and the transversus abdominis muscle (between the 2nd and 3rd muscle layers). The internal oblique muscle is usually the thickest muscle layer.
Selection of Local Anesthetic for Ilioinguinal Block
| Local anesthetic agent | Volume (ml) | Onset time | Duration |
|---|---|---|---|
| Mepivacaine 10 mg/ml | 20-40 ml (20 ml on each side) | 10-20 min | 2-5 hours |
| Ropivacaine 5 mg/ml | 15-20 ml | 10-45 min | 3-9 hours |
| Ropivacaine 7,5 mg/ml | 10-20 ml | 10-45 min | 3-9 hours |
| Bupivacaine 3,75 mg/ml | 15-20 ml | 15-30 min | 5-15 hours |
Warning: More challenging on obese patients. A pillow under the hip can help. Avoid puncturing through the peritoneum.
Video Link: https://www.youtube.com/watch?v=e1PemJ5lDrM
https://www.youtube.com/watch?v=gTJ6IrhVqwo
Infiltration Anesthesia
Indication: Local anesthesia cutaneously and subcutaneously where the local anesthesia is injected. For minor surgery or postoperative pain relief.
Infiltration anesthesia with local anesthetics
| Local anesthetic agent | Concentration | Volume (ml) | Dose (mg) | Brand name |
|---|---|---|---|---|
| Mepivacaine | 10 mg/ml | 1–20 ml | 10–200 mg | Carbocaine (Carbocaine®) |
| Lidocaine | 10 mg/ml | 5-40 ml | 50-400 mg | Xylocaine (Carbocaine®) |
| Levobupivacaine | 2,5–5 mg/ml | 1–20 ml | 2,5–100 mg | Chirocaine (Carbocaine®) |
| Prilocaine | 5 mg/ml | 1-20 ml | 5-100 mg | Citanest (Carbocaine®) |
Infraclavicular Plexus Block
Indication: Surgery on the upper arm, elbow, forearm, or hand.
Patient Position: Supine position with the arm elevated and abducted. The anesthesiologist can sit either below or above the patient’s shoulder. It may be advantageous to have an assistant perform the LA injection as three hands are practically required for the block. If seated above the patient’s shoulder, the insertion is best made from the top of the probe (cephalad).
Technique: Preferably use the In plane technique with insertion from the lateral side of the ultrasound probe. Insert the needle under the probe parallel to the probe head’s longitudinal axis. The target for the needle tip is the nerves around the artery. Perform as few injections as possible, preferably 2-3, deep and lateral to the artery, possibly also medially. Ideal spread is around the hyperechoic nerve root structures, about 5-10 ml in each spot. Note hydrodissection, i.e., filling with anesthetic fluid (LA). Proper hydrodissection typically causes a brief compression of the artery. The injection needle is more visible with the In plane technique than with the Out of plane technique.
Transducer: 10-16 MHz, linear probe (“Hammerhead”).
Probe Position: In plane (longitudinal) just below the clavicle. The probe can be positioned in a cephalad-caudal direction (probe head aligned with the body’s longitudinal axis). Insertion from the top (cephalad side).
Injection Needle: 21-22G, 8-10 cm long, bevel tip.
Nerve Stimulation Response: Hand.
Set Depth in Ultrasound Image: 5 cm.
Ideal Image: In plane (over a. axillaris): Displays the axillary artery as a pulsating hypoechoic sphere. Insertion is made from the cephalad side (center of the short side) of the probe head. The needle tip is placed laterally, medially, and under the artery.
Note the Anatomy: The pectoralis major muscle is on top. The artery lies under the fascia of the pectoralis minor muscle, which should be identifiable with ultrasound. The axillary vein (subclavian vein) lies just medial and caudal to the artery and is usually larger. Three nerve structures (medial, lateral, and posterior branches of the axillary plexus) can be identified around the artery as hyperechoic zones, typically with the medial branch at 2-3 o’clock, the posterior branch at 4-5 o’clock, and the lateral branch at 6-7 o’clock if the artery is imagined as a clock face. Anatomical variations occur.
Selection of local anesthetic for Infraclavicular Plexus Block
| Local anesthetic agent | Volume (ml) | Onset time | Duration |
|---|---|---|---|
| Mepivacaine 10 mg/ml | 10-30 ml | 10-20 min | 2-5 hours |
| Ropivacaine 5 mg/ml | 20-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 7,5 mg/ml | 10-20 ml | 10-45 min | 3-9 hours |
| Lidocaine 10 mg/ml | 20-30 ml | 10-20 min | 1-4 hours |
Warning: Avoid puncturing the brachial artery or brachial vein. Do not inject directly into the nerves; observe any resistance to injection. In case of accidental arterial puncture, withdraw the needle and apply firm pressure for 3-5 minutes. Then repeat the needle insertion under better visualization, with the In plane technique. Avoid puncturing into the nerve roots, which results in resistant injection.
Video Link: https://www.youtube.com/watch?v=hRyDtXrfYqc
Interscalene Block
Indication: Surgery on the shoulder, distal clavicle, proximal humerus.
Patient Position: Supine or semi-sitting or lateral position.
Technique: Use the In plane technique with insertion from the lateral side of the ultrasound probe. The probe should be slightly angled towards the jugulum. Insert the needle under the probe parallel to the probe’s longitudinal axis. The target for the needle tip is the interscalene space (groove-spatium). Perform as few injections as possible, preferably 2-3. Ideal spread is between ASM and MSM around the hypoechoic nerve root structures. If it is difficult to visualize the nerve root structures, start scanning directly above the clavicle and move 3-5 cm upwards in a cranial direction.
Transducer: 10-16 MHz, linear probe (“Hammerhead”).
Probe Position: Over v. jugularis externa, about 3 cm above the clavicle.
Injection Needle: 22G, 5 cm long, bevel tip.
Nerve Stimulation Response: Shoulder, arm, forearm.
Set Depth in Ultrasound Image: 3 cm.
Ideal Image: 2-3 branches of the nerve tree visible in the image.
Note the Anatomy: Visualize the scalene anterior (msa) and medius (msm) muscles. 2-3 hypoechoic structures correspond to the interscalene nerve branches.
Selection of local anesthetic for Interscalenius Block
| Local anesthetic agent | Volume (ml) | Onset time | Duration |
|---|---|---|---|
| Mepivacaine 10 mg/ml | 10-20 ml | 10-20 min | 2-5 hours |
| Ropivacaine 5 mg/ml | 5-20 ml | 10-45 min | 3-9 hours |
| Ropivacaine 7,5 mg/ml | 5-15 ml | 10-45 min | 3-9 hours |
| Lidocaine 10 mg/ml | 10-20 ml | 10-20 min | 1-4 hours |
Warning: Avoid puncturing the vertebral artery. Caution with patients with advanced COPD, lung emphysema, and/or dyspnea.
Video Link: https://www.youtube.com/watch?v=h_30mwMLH6M
Local Anesthetic Systemic Toxicity (LAST)
- Rare but serious, caused by overdose of local anesthetic.
- Treated with antidote (Intralipid®) (see below)
Symptoms:
- Mild: dizziness, metallic taste, numb lips/tongue, tinnitus.
- Moderate: disorientation, reduced consciousness.
- Severe: hypotension, bradycardia, unconsciousness, seizures, respiratory arrest, arrhythmia, asystole.
Treatment:
- Stop local anesthetic infusion and ALERT anesthesia immediately.
- Give 10 L oxygen via OxyMask.
- Apply monitoring (POX, ECG, BP).
- In cardiac arrest, start CPR.
- In cardiovascular collaps – give Intravenous Lipid Emulsion Therapy
If LAST is suspected, regardless of severity, stop infusion and contact anesthesiologist immediately.
Intravenous Lipid Emulsion Therapy
In the event of circulatory arrest, CPR should be performed immediately and lipid therapy should be attempted.
Administer a bolus of a 20% lipid emulsion Intralipid 1 ml/kg IV or 100-200 ml quickly intravenously. Start an infusion with the same lipid emulsion 0.25 ml/kg/min for 10 minutes, during which CPR is performed, or an additional 100 ml intravenously. Bolus doses may be repeated every 5 minutes, two or three times if needed, 1 ml/kg Intralipid. No more than 12 ml/kg lipid emulsion should be given.
Blood sampling: Arterial blood gas with acid-base status, frequent electrolyte checks (routine status), P-glucose. Further treatment is guided by the patient’s condition. Prolonged CPR may be needed in toxic reactions to Marcaine (bupivacaine) with high toxicity and a high apparent volume of distribution (Vd).
Nerve Block on Fingers and Toes
Indication: Local anesthesia of fingers or toes
Nerve block on fingers and toes
| Local anesthetic agent | Concentration | Volume (ml) | Onset Time | Duration | Dose (mg) | Drug |
|---|---|---|---|---|---|---|
| Lidocaine | 10 mg/ml | 2–4 ml | 1-5 min | 1-4 hours | 20–40 mg | Xylocaine® |
| Mepivacaine | 10 mg/ml | 2–5 ml | 1-5 min | 2-5 hours | 20–50 mg | Carbocaine ® |
| Mepivacaine | 20 mg/ml | 1-5 ml | 1-5 min | 2-5 hours | 20-100 mg | Carbocaine® |
| Prilocaine | 5 mg/ml | 1-5 ml | 1-5 min | 1-2,5 hours | 5-25 mg | Citanest® |
Paravertebral Block
Indication: Anesthesia or pain releif after thoracic procedures such as chest surgery or breast surgery. Anesthesia level at Th2-Th6.
Patient Position: Sitting or lying on the side.
Technique: Angle the lower part of the probe parallel to the medial edge of the scapula. Use the In plane technique with insertion 0.5 cm from the lateral side (caudal end) of the ultrasound probe’s head. Insert the needle under the probe’s head laterally to the target. Identify the space between the fourth and fifth ribs. The ribs appear as rounded large densities. Between and under these lie the internal intercostal muscle and underneath the pleura. The ideal spread of the local anesthetic is between the internal intercostal muscle and the pleura. Penetrate the upper costotransverse membrane (superior costotransverse ligament) under the internal intercostal muscle. Perform as few injections as possible, preferably only one.
Note proper hydrodissection, i.e., filling the space between the internal intercostal muscle and pleura. The pleura should ideally bulge downward from hydrodissection during the injection itself.
Transducer: 8-16 MHz, linear probe.
Probe Position: Place the probe in a vertical direction (paramedian position) about 5 cm to the side of the spine towards the upper part of the back.
Injection Needle: 20 G, 8 cm long, bevel tip.
Nerve Stimulation Response: None.
Set Depth in Ultrasound Image: 3 cm.
Ideal Image: Th 4-Th 5. Visualize the first rib, then the second, third, and fourth ribs. Visualize two transverse processes, then the internal intercostal muscle between them, and pleura underneath.
Note the Anatomy: Trapezius muscle, rhomboideus minor muscle, rhomboideus major muscle. Transverse processes, fourth and fifth ribs. Internal intercostal muscle. Pleura. The paravertebral space to be reached is located just above the pleura at the level of the foot (lower part) of the adjacent transverse process (like a flat area at the foot of two hills).
Selection of local anesthetic agent for Paravertebral Block
| Local anesthetic agent | Volume (ml) | Onset time | Duration |
|---|---|---|---|
| Mepivacaine 10 mg/ml | 20-40 ml (20 ml on each side). | 10-20 min | 2-5 hours |
| Ropivacaine 5 mg/ml | 15-20 ml unilaterally or 30-40 ml to 2 sides. | 10-45 min | 3-9 hours |
| Ropivacaine 7,5 mg/ml | 10-20 ml unilaterally or 20-30 ml to 2 sides | 10-45 min | 3-9 hours |
| Bupivacaine 5 mg/ml | 15-20 ml unilateral (not bilateral) | 15-30 min | 5-15 hours |
Warning: More challenging in obese patients. The sitting position is preferred, but compromised patients or those heavily influenced by pharmacology should lie on their side. Obviously, avoid puncturing through the pleura. Avoid bilateral block due to the risk of bilateral pneumothorax. An assistant should monitor the patient from the front. Aspirate before injection. Use small repeated doses during the block.
Video Link: https://www.youtube.com/watch?v=tFfetJitDrk
PECS I and II Block
Indication: Breast surgery. Thoracic wall surgery. Anesthesia of n. pectoralis medialis, n. pectoralis lateralis, and superficial intercostal nerve branches.
Patient Position: Supine position.
Ideal Image: Local anesthesia is injected in two points:
A) The first injection of about 0.2 ml/kg long-acting local anesthetic is made between the pectoralis major and pectoralis minor muscles.
B) The second injection of 0.2 ml/kg is made between the pectoralis minor and serratus anterior muscles. The figure below illustrates the sonographic anatomy, needle path, and desired injection spread.
Transducer: 10-16 MHz, linear probe (“Hammerhead”).
Set Depth in Ultrasound Image: 3-5 cm.
Probe Position: In plane technique (with the probe in a transverse or longitudinal position).
Injection Needle: 22G, 8 cm long, bevel tip.
On the pectoral level, the muscle fasciae create four potential spaces for the injection of local anesthesia:
- Between the superficial and deep pectoral muscle fascia.
- Between the pectoral fascia and the clavipectoral fascia.
- Between the clavipectoral fascia and the superficial edge of the serratus anterior muscle.
- Between the serratus anterior muscle and the extrathoracic fascia.
Selection of local anesthetic agent for PECS-II-Block
| Local anesthetic agent | Concentration | Volume (ml) | Onset time | Duration |
|---|---|---|---|---|
| Mepivacaine 1% | 10 mg/ml | 20-40 ml | 10-20 min | 2-5 hours |
| Ropivacaine 0.5% | 5 mg/ml | 20-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 0.75% | 7,5 mg/ml | 10-20 ml | 10-45 min | 3-9 hours |
| Lidocaine 1% | 10 mg/ml | 20-30 ml | 10-20 min | 1-4 hours |
| Bupivacaine 0.25% | 2,5 mg/ml | 30 ml | 15-30 min | 5-15 hours |
Warning:
Video Link: https://www.youtube.com/watch?v=YFWneF4pwOA
Continuous Peripheral Nerve Block (PNB) – Checks
Standard Checks
Checks in the ward
Date
Time
Signature
Vital signs
- Respiratory rate /min
- SpO₂ / O₂ % L
- Pulse /min
- Blood pressure mmHg
Neurology
- Pain at rest/mobilization (NRS 0–10)
- Sensory function (Yes/No)
- Motor function (Yes/No)
- Anxiety
Other
- Functioning peripheral venous catheter (PVC)
PNB – INFUSION
Medication: Ropivacaine 2 mg/ml
Settings:
- Continuous (plexus block)
- Intermittent (fascia block)
- Daily dose mg
- Clinician bolus mg
- Total amount administered mg/day
Insertion site normal/remarks — once daily
At initiation
- Continuous monitoring with 3‑lead ECG, pulse oximetry, blood pressure measurement, and general neurological assessment.
- Ensure functioning IV access.
- If the block is placed without complications, monitor the patient for 30 minutes.
On the ward:
- Checks every 4 hours, may be extended to every 6 hours after one day without dose increase.
Extra checks
- After clinician bolus beyond the programmed infusion: extra checks after 10 and 30 minutes.
- After catheter adjustment on the ward or infusion program changes: extra checks after 10 and 30 minutes.
Complications
Complications are uncommon and vary with block type. General risks include infection, bleeding, nerve injury, and LAST.
Discontinuation
- Consider discontinuation after four days due to increasing infection risk.
- Coagulation tests are not needed before discontinuation.
Popliteal Block
Indication: Surgery or pain conditions in the ankle, instep, or foot. Block of sciatic nerve in the popliteal fossa or just above it.
Patient Position: Lateral, prone, or semi-prone lateral position.
Technique: Use the In plane technique with insertion from the lateral side of the ultrasound probe’s head. Insert the needle under the probe laterally to the target. The target for the needle tip is Sciatic nerve; the needle must enter within the tendon sheath. Perform as few injections as possible, preferably 2, one on each side of the nerve, at about 2 cm depth. Ideal spread is around the hyperechoic nerve root structure of the sciatic nerve or between n. peroneus communis and tibial nerve. Note hydrodissection, i.e., filling around the nerve with LA.
When using the Out of plane technique, the needle should enter the image vertically in the midline.
Transducer: 8-16 MHz, linear probe.
Probe Position: Transverse, about 4-5 cm above the knee joint, at the base of the popliteal fossa.
Injection Needle: 22G, 5-8 cm long, bevel tip.
Nerve Stimulation Response: Foot or toe.
Set Depth in Ultrasound Image: 4 cm.
Ideal Image: Visualize the sciatic nerve division into n. peroneus communis and tibial nerve about 5 cm above the knee joint. The “snowman” should be visible in the image.
Note the Anatomy: Popliteal artery. Femur. The sciatic nerve lies above and lateral to the vein and artery; note the tendon sheath that the sciatic nerve lies in. Semitendinosus muscle.
Selection of local anesthetic for Popliteal Block
| Local anesthetic agent | Concentration | Volume (ml) | Onset time | Duration |
|---|---|---|---|---|
| Mepivacaine 1% | 10 mg/ml | 20-30 ml | 10-20 min | 2-5 hours |
| Ropivacaine 0,5% | 5 mg/ml | 20-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 0,75% | 7,5 mg/ml | 15-25 ml | 10-45 min | 3-9 hours |
| Lidocaine 1% | 10 mg/ml | 20-30 ml | 10-20 min | 1-4 hours |
| Bupivacaine 0.25% | 2,5 mg/ml | 20-30 ml | 15-30 min | 5-15 hours |
Warning: Follow the nerve’s distribution and division. The block can also be placed slightly higher up. If a continuous catheter is placed, it must be within the tendon sheath. It takes about 30 minutes to take full effect.
Video Link: https://www.youtube.com/watch?v=kzhSiQBPE7s
Rectus Block (Rectus Sheath Block, Paraumbilical Block)
Indication: Abdominal wall incision in the midline. Exploratory laparotomies, abdominal wall hernia surgery, hysterectomy, Bricker deviation.
Patient Position: Supine position.
Technique: Use the In plane technique with the probe horizontal and insertion 0.5 cm lateral to the ultrasound probe. Locate the image with the needle, reach the space between the RM and the “railroad track” with the needle in the image. Hydrodissect to ensure placement—fluid spread side to side on the ultrasound screen. The rectus block needs to be placed bilaterally except in exceptional cases.
Transducer: 8-16 MHz, linear probe.
Probe Position: At the cranial part of the incision or just above it. The probe is placed horizontally superficial to the lateral aspect of the rectus muscle (RM). Insert in-plane. Alternatively, rotate with RM in the image, the probe sagittally to inject cranially-caudally, about 2 cm medial to the linea semilunaris.
Injection Needle: 20-22 G, 5 cm long, bevel tip.
Set Depth in Ultrasound Image: 4 cm initially.
Ideal Image: With the probe horizontal, the rectus muscle is clearly visible between subcutaneous fat and a deeper “railroad track.” At the lateral edge of the muscle, the transversus abdominis muscle (TAM) may extend deeply towards the medial rectus muscle. Deep to the “railroad track” lies the peritoneum, and bowel movements may be seen.
Note the Anatomy: The “railroad track” consists of the posterior rectus sheath (the aponeurosis of TAM and the posterior lamina of the internal oblique muscle aponeurosis) and the transversalis fascia (deeper, towards the peritoneum). The T6/7-T12 nerves lie between the posterior rectus sheath and the RM up to about 2 cm from the RM’s lateral edge, from where they penetrate the RM, anastomose cranially/caudally, and penetrate to the skin. Vascular branches from the superior/inferior mesenteric arteries are located more medially. The rectus sheath is not adherent to the muscle except after previous complicated surgery, and the local anesthetic spreads very well in the layer. At the linea arcuata below the navel, the posterior rectus sheath lies superficial to the RM. The abdominal wall is supplied caudally from here by the iliohypogastric and ilioinguinal nerves (L1), which perforate superficially already laterally to the RM.
Warning: The duration with long-acting local anesthetics is only about 6-8 hours after a single shot dose. With indwelling catheters bilaterally, dosing every 4 hours is necessary. 20 ml per side. Avoid toxic doses or puncturing the peritoneum.
Video Link: https://www.youtube.com/watch?v=WOyTeZK4Ys8
Saphenous Block
Indication: Addition to popliteal or sciatic nerve block for surgery below the knee. Block of saphenus nerve.
Patient Position: Supine position, with the leg abducted, externally rotated, and slightly flexed at the knee.
Technique: Use the In plane technique with insertion from the lateral side of the ultrasound probe’s head. Insert the needle under the probe laterally to the target. The target for the needle tip is Saphenus nerve lateral to the femoral artery under the sartorius muscle. Perform as few injections as possible, preferably only one. Ideal spread is around the hyperechoic nerve root structure of the saphenous nerve or around and under the femoral artery. Note hydrodissection, i.e., filling around the nerve with LA. The saphenous block can also be placed below the knee joint on the lateral side.
Transducer: 8-16 MHz, linear probe.
Probe Position: Transverse position, about 10 cm above the knee joint on the lateral (front) side of the thigh.
Injection Needle: 22G, 8 cm long, bevel tip.
Nerve Stimulation Response: Medial part of the lower leg and calf.
Set Depth in Ultrasound Image: 4-6 cm.
Ideal Image: Visualize the femoral artery. Saphenus nerve lies anterior (lateral) to the femoral artery under the sartorius muscle.
Note the Anatomy: Femur, femoral artery. Saphenus nerve may be difficult to visualize. Vastus medialis muscle. Sartorius muscle.
In the Out of plane technique, the needle should enter the image vertically in the midline.
Selection of local anesthetic for Saphenus Block
| Local anesthetic agent | Concentration | Volume (ml) | Onset time | Duration |
|---|---|---|---|---|
| Mepivacaine 1% | 10 mg/ml | 10-20 ml | 10-20 min | 2-5 hours |
| Mepivacaine 2% | 20 mg/ml | 5-10 ml | 10-20 min | 2-5 hours |
| Ropivacaine 0,5% | 5 mg/ml | 10 ml | 10-45 min | 3-9 hours |
| Ropivacaine 0,75% | 7,5 mg/ml | 5-10 ml | 10-45 min | 3-9 hours |
| Lidocaine 1% | 10 mg/ml | 10-20 ml | 10-20 min | 1-4 hours |
Warning: Follow the nerve’s distribution and division. Saphenus nerve can be difficult to visualize.
Video Link: https://www.youtube.com/watch?v=rn1pI48D3Ik
Sciatic Nerve Block
Indication: Surgery or pain conditions in the knee or knee joint region. Anesthesia of sciatic nerve.
Patient Position: Prone, lateral, or semi-prone lateral position.
Technique: Use the In plane technique with insertion 3-4 cm from the lateral side of the ultrasound probe’s head. Insert the needle under the probe laterally to the target. The target for the needle tip is Sciatic nerve; the needle must enter within the sheath. Perform as few injections as possible, preferably 2, one injection on each side of the nerve. Ideal spread is around the hyperechoic nerve root structure. Note hydrodissection, i.e., filling around the nerve with LA. You may need to press the probe quite firmly against the patient’s thigh.
Transducer: 6-16 MHz, linear probe or curved probe for larger patients (“abdominal probe”).
Probe Position: Subgluteal.
Injection Needle: 21G, 10 cm long, bevel tip.
Nerve Stimulation Response: Foot or calf.
Set Depth in Ultrasound Image: 5 cm or more, varies with patient size.
Ideal Image: Visualize sciatic nerve and the epineural sheath.
Note the Anatomy: Sciatic nerve lies directly under the gluteus maximus muscle and above the quadratus femoris muscle. Trochanter major. Ischial tuberosity. Triangular nerve structure.
Choice of local anesthetic for Sciatic Block
| Drug | Local anesthetic agent | Volume (ml) | Onset time | Duration |
|---|---|---|---|---|
| Mepivacaine 1% | Mepivacaine 10 mg/ml | 20-30 ml | 10-20 min | 2-5 hours |
| Ropivacaine 0,5% | Ropivacaine 5 mg/ml | 20-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 0,75% | Ropivacaine 7,5 mg/ml | 10-20 ml | 10-45 min | 3-9 hours |
| Xylocain 1% | Lidocaine 10 mg/ml | 20-30 ml | 10-20 min | 1-4 hours |
Warning: The puncture may be relatively deep, making it difficult to visualize sciatic nerve in obese patients.
Video Link: https://www.youtube.com/watch?v=rl8rZOEMveE
Serratus Plane Block
Indication: Thoracic wall surgery.
Patient Position: Lateral or with the arm forward is preferred.
Technique: There are two main methods to identify the site for the serratus block. The first method requires counting the ribs from the clavicle while moving the probe laterally and distally until the fourth and fifth ribs can be identified (see figure). The probe should be oriented in the horizontal plane and then tilted backward until the latissimus dorsi muscle (a superficial thick muscle) can be identified. The serratus anterior muscle, a thick, hypo-echoic structure, lies deep to the latissimus dorsi muscle, which is imaged over the ribs. If the probe is directed backward, it allows identification of the plane between the serratus anterior muscle and the latissimus dorsi muscle. An alternative method is to place the probe over the axilla, where the latissimus dorsi muscle will appear more clearly (see Figure). The positioning of the thoracodorsal artery is easier to identify this way. Both In-plane and Out-of-plane methods are suitable for puncture.
Transducer: 10-16 MHz, linear probe (“Hammerhead”).
Probe Position: In plane technique (in transverse or longitudinal position) or Out-of-plane.
Injection Needle: 22G, 8 cm long, bevel tip.
Nerve Stimulation Response: .
Set Depth in Ultrasound Image: 2.5-3 cm.
Ideal Image: The serratus plane block is performed in the axillary region but more laterally and dorsally compared to the PECS I and II blocks. At the axillary fossa lies the intercostobrachial nerve, as well as the lateral cutaneous branches of the intercostal nerves (T3-T9), the long thoracic nerve, and the thoracodorsal nerve, which are located in a compartment between the serratus anterior muscle and the latissimus dorsi muscle, between the posterior and midaxillary lines.
Note the Anatomy: The two main anatomical landmarks are the latissimus dorsi and serratus anterior muscles. The thoracodorsal artery runs in the fascial plane between the two muscles. Ribs, pleura, and intercostal muscles can also be seen during the procedure.
Selection of local anesthetic for Serratus Plane Block
| Local anesthetic agent | Concentration | Volume (ml) | Onset time | Duration |
|---|---|---|---|---|
| Mepivacaine 1% | 10 mg/ml | 20-40 ml | 10-20 min | 2-5 hours |
| Ropivacaine 0,5% | 5 mg/ml | 15-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 0,75% | 7,5 mg/ml | 15-20 ml | 10-45 min | 3-9 hours |
| Bupivacaine 0.375% | 3.75 mg/ml | 15 ml | 15-30 min | 5-15 hours |
| Lidocaine 1% | 10 mg/ml | 20-40 ml | 10-20 min | 1-4 hours |
Video Link: Click here for link
Supraclavicular Plexus Block
Indication: Surgery on the humerus, elbow, hand.
Patient Position: Supine or semi-lateral position. Slight head rotation to the opposite side. Slightly elevated head.
Technique: Use the In-plane technique with insertion on the lateral side of the ultrasound probe. Insert the needle under the probe parallel to the probe’s length. The goal for the needle tip is inside the plexus sheath lateral to the subclavian artery and above the first rib. Perform as few injections as possible, preferably 2-3. Ideal spread is around the hyper-echoic nerve root structures. If it is difficult to visualize the nerve root structures, start scanning directly above the clavicle. Note hydrodissection, i.e., plexus sheath filling with LA.
In courtesy of NYSORA
Transducer: 10-16 MHz, linear probe (“Hammerhead”).
Probe Position: In the supraclavicular fossa. Lateral to the clavicular head, in a cephalad-caudal direction.
Injection Needle: 22G, 5 cm long, bevel tip.
Nerve Stimulation Response: Arm, forearm.
Set Depth in Ultrasound Image: 3 cm.
Ideal Image: Brachial plexus and subclavian artery above the first rib and pleura.
Note the Anatomy: Subclavian artery. First rib. Pleura. The nerve plexus has a honeycomb pattern that is both hypo-echoic and hyper-echoic, lying immediately lateral to the subclavian artery and medial to the middle scalene muscle (msm). The nerve roots are typically hypo-echoic.
Choice of local anesthetic for Supra Clavicular Plexus Block
| Local anesthetic agent | Concentration | Volume (ml) | Onset Time | Duration |
|---|---|---|---|---|
| Mepivacaine 1% | 10 mg/ml | 20-30 ml | 10-20 min | 2-5 hours |
| Ropivacaine 0,5% | 5 mg/ml | 20-30 ml | 10-45 min | 3-9 hours |
| Ropivacaine 0,75% | 7,5 mg/ml | 10-20 ml | 10-45 min | 3-9 hours |
| Bupivacaine 0.375% | 3.75 mg/ml | 20-30 ml | 15-30 min | 5-15 hours |
| Lidocaine 1% | 10 mg/ml | 20-30 ml | 10-20 min | 1-4 hours |
Warning: Avoid puncturing the pleura and subclavian artery. Caution with patients with advanced COPD, pulmonary emphysema, or dyspnea.
Video Link: https://www.youtube.com/watch?v=ztOIvfjsB-U
Suprazygomatic Maxillary Block
Indication: Palate surgery, tooth extraction, possible jaw surgery in the maxillary area.
Patient Position: Supine
Technique: The needle is inserted perpendicular to the skin approximately 1 cm lateral to the lateral orbital rim, above the zygomatic arch, to bone contact at a depth of 1-2 cm (sphenoid wing). The needle is then slightly retracted and redirected towards the philtrum (the groove between the upper lip and nose) and advanced 35-45 mm (possibly slightly longer in adults). A “pop” or release may be felt as the needle exits the masseter muscle into the pterygopalatine fossa but is not always felt.
Transducer: Hockey stick probe for children, linear probe for adults.
Probe Position: Below the zygomatic arch.
Injection Needle: 25-27 G, 40-50 mm (preferably the longer one for adults)
Nerve Stimulation Response: Twitching of the masseter muscle, which ceases when the needle tip exits the muscle into the pterygopalatine fossa.
Ideal Image: The nerve and needle are difficult to visualize in the image, but the maxillary artery can be seen, and the spread of local anesthetic in the area around the artery.
Selection of local anesthetic for Suprazygomatic Maxillary Block
| Local anesthetic agent | Concentration | Volume (ml) | Onset time | Duration |
|---|---|---|---|---|
| Ropivacaine 0,2% | 2 mg/ml | 0,15 ml/kg | 10-45 min | 3-9 hours |
| Levobupivacaine 0,25% | 2,5 mg/ml | 0,15 ml/kg | 15-30 min | 5-15 hours |
| Lidocaine 2% | 20 mg/ml | 3 ml to adults | 10-20 min | 1-4 hours |
Warning: Careful aspiration is essential as the maxillary artery runs caudally to the nerve. Injection should be smooth; resistance suggests the needle may be within the nerve.
Video Link: See above
References:
- Chiono, J., et al. “Bilateral Suprazygomatic Maxillary Nerve Block for Cleft Palate Repair in Children: A Prospective, Randomized, Double-Blind Study Versus Placebo.” Anesthesiology 120, no. 6 (Jun 2014): 1362-9.
- Mesnil, M., et al. “A New Approach for Peri-Operative Analgesia of Cleft Palate Repair in Infants: The Bilateral Suprazygomatic Maxillary Nerve Block.” Paediatr Anaesth 20, no. 4 (Apr 2010): 343-9.
- Radder, K., et al. “Efficacy and Feasibility of Frontozygomatic Angle Approach for Extra Oral Maxillary Nerve Block in Oral Surgery: A Descriptive Clinical Trial.” J Maxillofac Oral Surg 13, no. 3 (Sep 2014): 231-7.
TAP Block (Transversus Abdominis Plane)
Indication: Lower abdominal surgery, gynecological or urological surgery. Hysterectomy, inguinal hernia.
Patient Position: Supine position. Arms abducted.
Technique: Use the In-plane technique with insertion 0.5 cm from the medial side of the ultrasound probe’s head. Insert the needle under the probe medially to the target. The target for the needle tip is the TAP space between the internal oblique muscle and the transversus abdominis muscle. Penetration of the posterior fascia may be felt as a “pop” or “loss.” Perform as few injections as possible, preferably only one. Ideal spread is under the posterior rectus sheath. Note proper hydrodissection, i.e., filling of the TAP. TAP block is best placed bilaterally.
Transducer: 8-16 MHz, linear probe.
Probe Position: Midway between the iliac crest and the lower rib cage just above the level of the umbilicus. The probe is placed in a transverse position parallel to the rib cage.
Injection Needle: 20-22 G, 10 cm long, bevel tip.
Nerve Stimulation Response: None.
Set Depth in Ultrasound Image: 4 cm
Ideal Image: Visualize the rectus muscle medially. The transversus abdominis muscle lies beneath the rectus muscle and under the internal oblique muscle, which in turn lies under the external oblique muscle. The rectus muscle lies medially and is moved out and away.
Note the Anatomy: The transversus abdominis muscle lies beneath the internal oblique muscle, which lies beneath the external oblique muscle. Above the external oblique muscle is abdominal fat. The Transversus Abdominis Plane (TAP) is located under the posterior rectus sheath. The nerves are located between the transversus abdominis muscle and the internal oblique muscle (between the 2nd and 3rd muscle layers).
Choice of local anesthetic for Transversus Abdominal Plane TAP Block
| Local anesthetic agent | Concentration | Volume (ml) | Onset Time (min) | Duration (hours) |
|---|---|---|---|---|
| Mepivacaine 1% | 10 mg/ml | 20-40 ml (20 ml on each side) | 10-20 min | 2-5 hours |
| Ropivacaine 0,5% | 5 mg/ml | 20-40 ml. (20 ml on each side) | 10-45 min | 3-9 hours |
| Bupivacaine 0.375% | 3.75 mg/ml | 5 ml unilaterally or 30 ml on 2 sides | 15-30 min | 5-15 hours |
Warning: More challenging in obese patients. A pillow under the hip can help. Avoid puncturing the peritoneum.
Video Link: https://www.youtube.com/watch?v=9TIHDn7uBZI
Thoracic Epidural Block (Ultrasound-Guided)
Indication: Upper laparotomies. Th6-Th12.
Patient Position: Sitting or lying in a lateral position.
Technique: Start in the midline, then angle the probe downward sagittally paramedian. First visualize two transverse processes, then the ligamentum flavum between two laminae (2-3 cm in). The dura lies just beneath. The distance to the ligamentum flavum can be measured with the ultrasound (usually 3-5 cm).
Use the In-plane technique with insertion paramedian about 1 cm from the midline. Continue using the Loss-of-resistance (LOR) technique. Insert the epidural needle under the probe’s head laterally to the target. Identify the space between two laminae. The spinous process appears as rounded hypo-echoic densities. Between and beneath these lies the ligamentum flavum between two laminae and beneath the dura. Note the distance between the ligamentum flavum and dura. Penetrate the ligamentum flavum using LOR. Perform as few injections as possible, preferably only one.
Transducer: 8-12 MHz, linear or curved probe.
Probe Position: Initially place the probe in a paramedian position centrally over the spine towards the upper back. Then angle the probe in a paramedian sagittal section.
Injection Needle: 18 G epidural Tuohy needle.
Nerve Stimulation Response: None.
Set Depth in Ultrasound Image: 5-8 cm.
Local Anesthetic: First, numb the skin locally with 2 ml Carbocain 1% or Xylocain 1%. For the epidural block itself, use, for example:
- Carbocain 10 mg/ml (1%) 6-10 ml.
- Narop 5 mg/ml (0.5%) 4-6 ml.
- Bupivacaine 5 mg/ml (0.5%) 4-6 ml.
Ideal Image: Th8-Th9, Th9-Th10, Th10-Th11. Visualize the spinous process in the midline, lamina, and transverse process, ligamentum flavum, and dura.
Note the Anatomy: Lamina, interlaminar space, ligamentum flavum, posterior dura, ribs, pleura.
Warning: More challenging in obese patients. The dura may be difficult to distinguish from the ligamentum flavum. The sitting position is preferred, but patients who are severely compromised or heavily pharmacologically influenced should lie in a lateral position. Avoid puncturing the dura. An assistant should monitor the patient from the front. Aspirate before injection. Use small, repeated doses during the block.
Continuous Epidural Analgesia for Postoperative Pain Relief
| Local anesthetic | Opioid | Adrenaline addition | Dosage |
|---|---|---|---|
| Bupivacaine 1,0 mg/ml | Fentanyl 2 μg/ml + | Adrenaline 2 μg/ml | 8-14 ml/hour (Breivik's blend/BFA) |
| Bupivacaine 2,5 mg/ml | Sufentanil 0,5 μg/ml | 8-12 ml/hour | |
| Bupivacaine 2,5 mg/ml | Morphine Special 0,4 mg/ml | 5-10 ml/hour | |
| Bupivacaine 1,0 mg/ml | Sufentanil 1 μg/ml | 8-16 ml/hour | |
| Ropivacaine 2 mg/ml | Sufentanil 1 μg/ml | 8-16 ml/hour | |
| Ropivacaine 2 mg/ml | Morphine Special 0,4 mg/ml | 5-10 ml/hour | |
| Levobupivacaine 1,25 mg/ml | Sufentanil 1 μg/ml | 8-16 ml/hour | |
| Levobupivacaine 1,25 mg/ml | Morphine Special 0,4 mg/ml | 5-10 ml/hour | |
Continuous epidural anesthesia without opioids | |||
| Bupivacaine 2,5 mg/ml | 5-7,5 ml/hour | ||
| Ropivacaine 2 mg/ml | 6-14 ml/hour | ||
| Levobupivacaine 1,25 mg/ml | 10-15 ml/hour | ||
| Levobupivacaine 2.5 mg/ml | 5-7,5 ml/hour | ||
Video Links:
- https://www.youtube.com/watch?v=RMFulhXbmYk
- https://www.youtube.com/watch?v=M4hiP46YMuc
- [https://www.youtube.com/watch?v=-lE6xMUXMu
Regional Anesthesia Pocket Guide
For quick access to essential regional anesthesia techniques, download the Regional Anesthesia Pocket Guide. This guide is a valuable resource for anesthesiologists and healthcare professionals, providing concise information and practical tips for a variety of regional blocks.
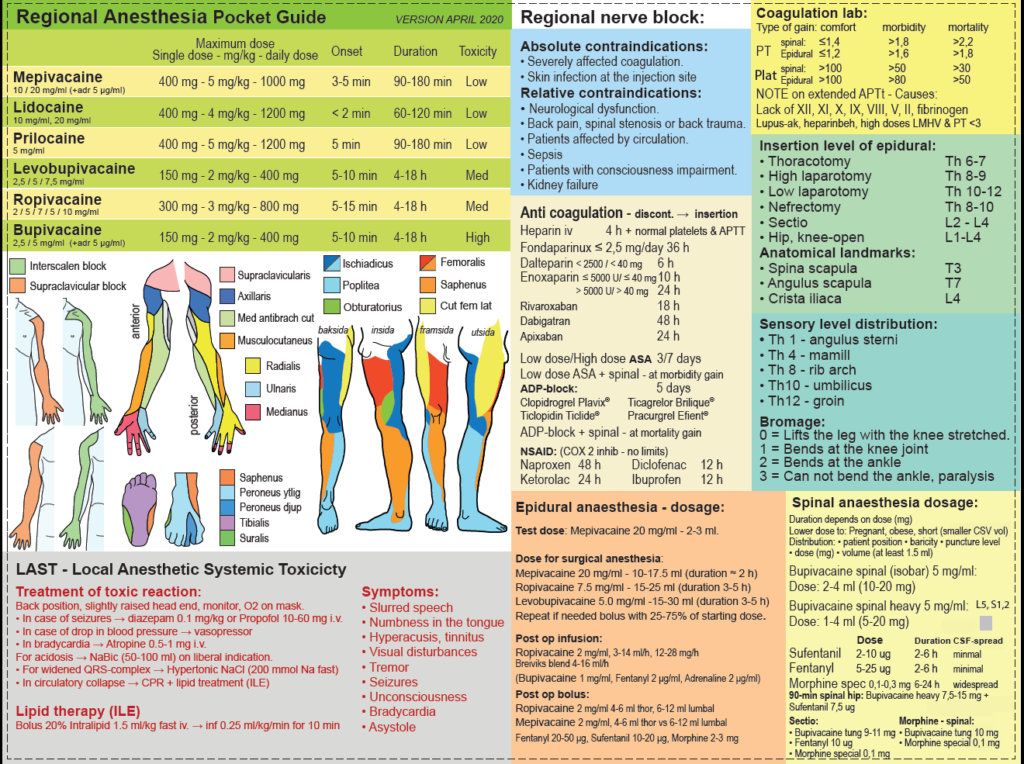
Click the image or here to download the guide.
Disclaimer:
The content on AnesthGuide.com is intended for use by medical professionals and is based on practices and guidelines within the Swedish healthcare context.
While all articles are reviewed by experienced professionals, the information provided may not be error-free or universally applicable.
Users are advised to always apply their professional judgment and consult relevant local guidelines.
By using this site, you agree to our Terms of Use.


