Author:
Kai Knudsen
Updated:
26 August, 2025
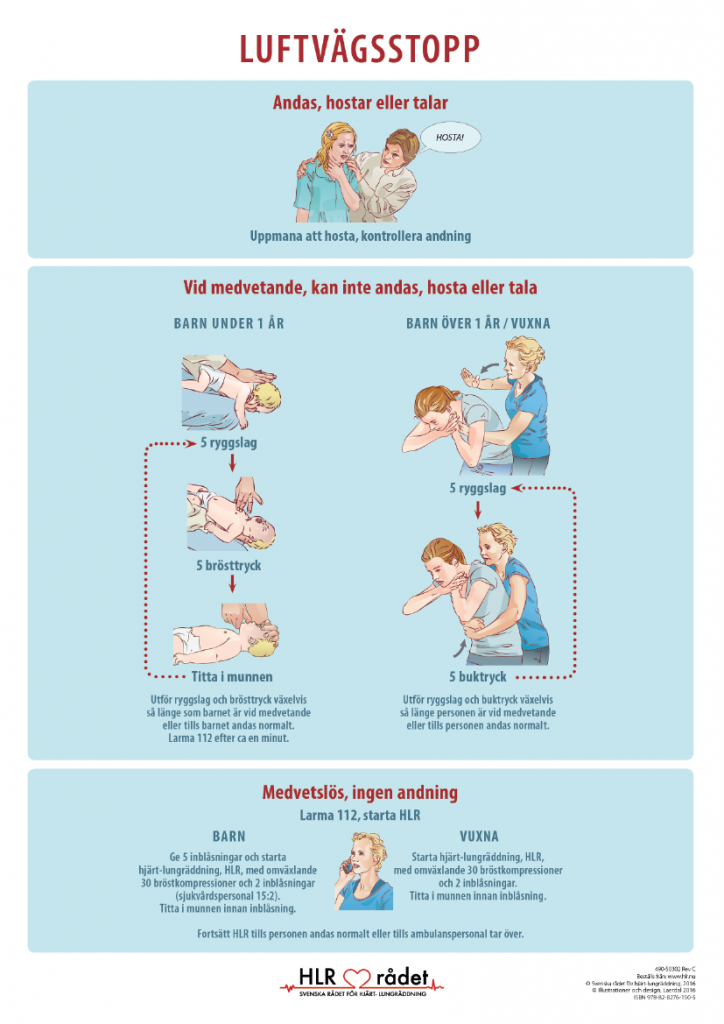
Here, guidelines for cardiopulmonary resuscitation (CPR) for children are described in accordance with the Swedish Heart-Lung Council. The graphical posters from the Swedish CPR Council are also available here, including those for airway obstruction in children.
CPR for Children
If there are no signs of life in the child: Start cardiopulmonary resuscitation (CPR) with five rescue breaths. For cardiac arrest in children, give five breaths immediately, then start CPR at a ratio of 15:2. Perform CPR for one minute before calling emergency services (112) if no one else has done so. Children rarely suffer from rhythm disorders; the most common cause of cardiac arrest in children is lack of oxygen. Then perform three cycles of 15 chest compressions and two breaths. Call emergency services. Continue CPR, alternating between 15 compressions and two breaths until help arrives or the child begins to breathe normally.

Primary CPR in Children
Secondary CPR in Children

Click the image to view the PDF version of the image.
Advanced CPR in Children
Medications at cardiac arrest in children
| Age | 0 | 3 months | 1 year | 5 years | 9 years | 12 years | 14 years | 15 years and older | |
|---|---|---|---|---|---|---|---|---|---|
| Weight | 3 kg | 5 kg | 10 kg | 20 kg | 30 kg | 40 kg | 50 kg | > 50 kg | |
| Epinephrine (0,1 mg/ml)* 0,01 mg/kg, 0,1 ml/kg | 0.3 | 0.5 | 1 | 2 | 3 | 4 | 5 | 10 | ml |
| Amiodarone (15 mg/ml)* 5 mg/kg, 0,33 ml/kg | 1 | 1.7 | 3 | 7 | 10 | 13 | 17 | 20 | ml |
| Glucose 100 mg/ml, 2 ml/kg | 6 | 10 | 20 | 40 | 60 | 80 | 100 | ml | |
| Ringer's Acetate 20 ml/kg | 60 | 100 | 200 | 400 | 600 | 800 | 1000 | ml | |
| Tribonate (0,5 mmol/ml) 2 ml/kg | 6 | 10 | 20 | 40 | 60 | 80 | 100 | 100 | ml |
| Defibrillation 4 J/kg | 12 | 20 | 40 | 80 | 120 | 150-200 | 150-200 | 150-360 | J |
| Endotracheal tube inner diameter | 3 | 3.5 | 4 | 5 | 6 | 7 | 7 | 7 | mm |
| *Amiodarone 50 mg/ml. 6 ml diluted with 14 ml glucose 50 mg/ml = 15 mg/ml | |||||||||
Performing CPR on Children
CPR should be continuous. Do not pause to check breathing or pulse. If possible, change the person performing compressions every two minutes. Stop CPR only if the child begins to breathe normally. Be mindful not to take too long between compressions and breaths.
Check in order: Consciousness, breathing, and signs of life. Does the child move, swallow, or breathe normally? Then provide the necessary aid.
- Is the child conscious? Call out to the child and gently pinch or shake their shoulders. If there is no response, shout for help from those nearby. Lay the child on their back.
- Is the child breathing? Open the airway. Look for movement in the chest and abdomen and check the child’s color. Listen for air flowing in and out through the mouth and nose. Feel the airflow on your cheek. If the child is breathing normally: place them in the recovery position. Continue to monitor the child’s breathing. Call for help. If the child is not breathing: give five slow rescue breaths. If you cannot blow air or the chest does not rise during breaths, there may be an obstruction in the child’s throat.
There are two ways to open the airway: Head-tilt/chin-lift. Gently tilt the child’s head back by placing one hand on the forehead. Lift the chin with the other hand’s index and middle fingers. For younger infants, avoid tilting the head too far back. Overextension of the head can block the airway. Jaw-thrust maneuver: Place one hand on the child’s forehead. Use the other hand’s thumb to grasp the lower jawline on younger infants or the lower teeth in children over one year. Use your index finger to support the chin, lifting it upward. Breaths: Infants (0-1 year): Perform the head-tilt/chin-lift. Cover the infant’s mouth and nose with your mouth. Blow air in slowly for 1-1.5 seconds, five times. Blow in enough air to see the chest rise and fall. Look for signs of life, movement, swallowing, or normal breathing during breaths.
Infants 0 to 1 Year
Place the baby on a firm surface. Start with five rescue breaths. Use your index and middle fingers to press the lower third of the breastbone. Press 15 times, almost two compressions per second. Each time, press the baby’s chest one-third of the depth. Release pressure between compressions. After 15 compressions, give two breaths. Then repeat, with 15 compressions followed by two breaths. If you are alone, call emergency services (112) after three cycles of 15 compressions and two breaths. Continue performing CPR, 15 compressions and two breaths, until help arrives or the baby starts breathing normally.
Management of airway obstruction in children

Neonatal CPR
Click the image to view the PDF version of the image.
Children 1 Year to Puberty
Pinch the child’s nostrils closed with your thumb and forefinger. Place your mouth over the child’s mouth and slowly blow air in for 1-1.5 seconds, five times. Blow in enough air to cause the chest to rise and fall. Look for signs of life, movement, swallowing, or normal breathing while giving breaths.
- Does the child show signs of life?
If the child shows signs of life but is not breathing normally: Give 20 breaths per minute and call 112. If you are alone, carry the child with you to the phone. Continue to give breaths. Around 20 breaths per minute is the recommended pace. If the child does not show signs of life: Perform cardiopulmonary resuscitation (CPR).
Medication During Ongoing CPR
For Asystole/Bradycardia/PEA
- Adrenaline 0.01 mg/kg immediately
- Repeat every four minutes
For VF/Pulseless VT
- Adrenaline 0.01 mg/kg after the third defibrillation. Repeat every four minutes.
- Amiodarone 5 mg/kg after the third defibrillation. Repeat the same dose after the fifth defibrillation.
Correct Reversible Causes
- Hypoxia
- Hypovolemia
- Hypothermia
- Hyper/hypokalemia
- Hypoglycemia
- Cardiac tamponade
- Tension pneumothorax
- Toxic conditions
- Thromboembolic events
CPR for Children

If there are no signs of life in the child: Start CPR with five rescue breaths. Then perform three cycles of 15 chest compressions and two breaths. Call for help. Continue CPR, alternating between 15 compressions and two breaths, until help arrives or the child starts breathing normally.
Advanced CPR for Children – Graphic Illustrations
Click the image to view the PDF version of the image.
Disclaimer:
The content on AnesthGuide.com is intended for use by medical professionals and is based on practices and guidelines within the Swedish healthcare context.
While all articles are reviewed by experienced professionals, the information provided may not be error-free or universally applicable.
Users are advised to always apply their professional judgment and consult relevant local guidelines.
By using this site, you agree to our Terms of Use.