Author:
Kai Knudsen
Updated:
27 August, 2025
This chapter outlines methods for grading consciousness, including clinical scales and assessment techniques used to evaluate neurological status
- Goal-Related Sedation
- Motor Activity Assessment Scale (MAAS Scale)
- Richmond Agitation-Sedation Scale (RASS)
- Ramsay Sedation Scale
- Nu-DESC The Nursing Delirium Screening Scale
- Riker Sedation-Agitation Scale (SAS)
- Confusion Assessment Method for the ICU (CAM-ICU)
- The Critical-Care Pain Observation Tool (CPOT)
- National Early Warning Score (NEWS)
- Glasgow Coma Scale (GCS)
- Glasgow Coma Scale
- Reaction Level Scale (RLS)
- Glasgow Coma Scale Children
- Focal Neurology
- NIH Stroke Scale
- Glasgow Outcome Scale
- Fisher Scale (modified) – SAH
- Hunt & Hess / WFNS grading
- CPC – Cerebral Performance Categories
- West Haven Scale for Grading Hepatic Encephalopathy
Goal-Related Sedation
Various scales are used to determine and observe patients’ alertness and level of consciousness in intensive care. Below, MAAS levels and RASS levels are presented. Increased sedation (low score) can increase the risk of respiratory and circulatory complications, while patient safety sometimes requires this.
A desired RASS level should be established daily for the individual patient after discussion within the care team. Often RASS 0 or −1. The doctor prescribes an appropriate RASS, e.g., −1. If the patient is then noted to correspond to RASS −3, the nurse turns off the sedative medication until the patient is again at RASS −2, after which sedation is restarted at a lower rate than before.
Motor Activity Assessment Scale (MAAS Scale)
The MAAS scale provides an assessment of alertness and comfort in ICU patients. Alertness is checked and documented every 3 hours in patients treated with a respirator, CPAP/noninvasive ventilation, or spontaneously breathing on a tube/tracheostomy. The MAAS scale is assessed as follows:
MAAS-Scale
| 0: | Unresponsive |
|---|---|
| 1: | Responsive only to noxious stimuli |
| 2: | Responsive to touch or name |
| 3: | Calm and Cooperative |
| 4: | Restless and cooperative |
| 5: | Agitated |
| 6: | Dangerously agitated, uncooperative |
Different MAAS levels are required for different patients. Increased sedation (low score) can increase the risk of respiratory and circulatory complications, while patient safety sometimes requires this.
We still know too little about patient comfort at different levels of sedation. New findings suggest that patients who clearly remember their intensive care experience fewer unpleasant memories (hallucinations, nightmares, paranoid thoughts) than those who do not remember as well. The RACHEL study found that patients who were kept deeply sedated for longer periods were more affected by hallucinations and nightmares.
Goal-Related Sedation
A desired MAAS level should be established daily for the individual patient after discussion within the care team. Often MAAS 2 or 3. The doctor prescribes an appropriate MAAS, e.g., 2. If the patient is then noted to correspond to MAAS 1, the nurse turns off the sedative medication until the patient is again at MAAS 2, after which sedation is restarted at a lower rate than before.
Richmond Agitation-Sedation Scale (RASS)
Richmond Agitation Sedation Scale RASS
| +4 | Combative: Overtly combative or violent, immediate danger to staff. |
|---|---|
| +3 | Very agitated: Pulling at or removing tubes/catheters, aggressive behavior towards staff. |
| +2 | Agitated: Frequent non-purposeful movements or fighting ventilator. |
| +1 | Restless: Anxious or apprehensive but with no aggressive or vigorous movements. |
| ±0 | Alert and calm. |
| -1 | Drowsy: Not fully alert but has sustained (more than 10 seconds) awakening, with eye contact in response to voice. |
| -2 | Light sedation: Briefly (less than 10 seconds) awakens with eye contact in response to voice. |
| -3 | Moderate sedation: Movement or slight response to voice, but no eye contact. |
| -4 | Deep sedation: No response to voice, but movement in response to physical stimulation. |
| -5 | Unarousable: No response to voice or physical stimulation. |
RASS is a validated tool for assessing mental parameters, allowing early identification of critical illness. It is documented every 3 hours in patients treated with a respirator, CPAP/noninvasive ventilation, or spontaneously breathing on a tube or tracheostomy.
Procedure for RASS Assessment
- Observe the patient. Is the patient alert and calm (0 points)? Does the patient exhibit behavior consistent with restlessness or agitation (points +1 to +4 using the criteria under the description)?
- If the patient is not alert, speak loudly to the patient and ask them to open their eyes and look at the speaker. Repeat once if necessary. Try to get the patient to continue looking at the speaker. The patient opens their eyes and maintains eye contact for more than 10 seconds (−1 point). The patient opens their eyes and maintains eye contact, but not for 10 seconds (−2 points). The patient makes some movement in response to the call, but no eye contact (−3 points).
- If the patient does not respond to verbal stimulation, physically stimulate the patient by shaking the shoulders and then rub the sternum if the response does not occur with shoulder shaking. The patient makes some movement with physical stimulation (−4 points). The patient gives no response to verbal or physical stimulation (−5 points).
Different RASS levels are required for different patients. Increased sedation (low score) can increase the risk of respiratory and circulatory complications, while patient safety sometimes requires this. We still know too little about patient comfort at different levels of sedation. New findings suggest that patients who clearly remember their intensive care experience fewer unpleasant memories (hallucinations, nightmares, paranoid thoughts) than those who do not remember as well. The RACHEL study found that patients who were kept deeply sedated for longer periods were more affected by hallucinations and nightmares.

Ramsay Sedation Scale
| Sedation Level | Score |
|---|---|
| Patient is anxious and agitated or restless, or both | 1 |
| Patient is co-operative, oriented, and tranquil | 2 |
| Patient responds to commands only | 3 |
| Patient exhibits brisk response to light glabellar tap or loud auditory stimulus | 4 |
| Patient exhibits a sluggish response to light glabellar tap or loud auditory stimulus | 5 |
| Patient exhibits no response | 6 |
Nu-DESC The Nursing Delirium Screening Scale
The majority of all ICU patients (up to 80%) suffer from delirium at some point during their ICU stay. Delirium means that one gets a distorted perception of reality in the form of confusion, hallucinations, and nightmares. This causes great suffering for the patients and leads to worse prognosis and longer hospital stays. There are three types of delirium: hyperactive, hypoactive, and a mixed state of these. A patient who is hyperactive, i.e., agitated and stressed, can be easily detected and diagnosed with delirium. However, it is more challenging to detect patients with hypoactive delirium, i.e., those who seem tired and do not communicate. The suffering and negative effects are just as severe. Therefore, it is important to detect and treat these patients.
Nu-DESC The Nursing Delirium Screening Scale
Grading of delirium symptoms with scoring as follows:
0: the symptom never occurs during the shift
1: the symptom occurs during part of the shift but is mild
2: the symptom occurs during part of the shift and is very pronounced or disruptive
Nu-DESC The Nursing Delirium Screening Scale
| Category | Symptom | Night Shift Score (0-2) | Morning Shift Score (0-2) | Evening Shift Score (0-2) |
|---|---|---|---|---|
| Disorientation/Confusion | Verbal or behavioral symptoms suggesting that the person is not oriented to time and place or confuses one person for another or misinterprets people in the surroundings. | |||
| Inappropriate Behavior | Inappropriate behavior in relation to the situation, such as pulling out cannulas, catheters, removing bandages, or attempting to get out of bed when contraindicated. | |||
| Inappropriate Communication | Inappropriate communication in relation to the situation, such as incoherent, incomprehensible, or meaningless speech. | |||
| Illusions/Hallucinations | Seeing or hearing things that do not exist, misperception/misinterpretation, or distortion of visual impressions. | |||
| Psychomotor Retardation | Delayed reaction, few or no spontaneous reactions or responses, for example, when stimulating the patient, no reaction (unable to wake up) or the reaction is significantly delayed. | |||
| Total: | Total: | Total: |
Definition of ICU delirium according to Nu-DESC is a total score of ≥ 2.
| Total: | Total: | Total: |
| 0: the symptom never occurs during the shift
1: the symptom occurs during part of the shift but is mild
2: the symptom occurs during part of the shift and is very pronounced or disruptive
Riker Sedation-Agitation Scale (SAS)
| Score | Term | Descriptor |
|---|---|---|
| 7 | Dangerous Agitation | Pulling at ET tube, trying to remove catheters, climbing over bedrail, striking at staff, thrashing side-to-side |
| 6 | Very Agitated | Requiring restraint and frequent verbal reminding of limits, biting ETT |
| 5 | Agitated | Anxious or physically agitated, calms to verbal instructions |
| 4 | Calm and Cooperative | Calm, easily arousable, follows commands |
| 3 | Sedated | Difficult to arouse but awakens to verbal stimuli or gentle shaking, follows simple commands but drifts off again |
| 2 | Very Sedated | Arouses to physical stimuli but does not communicate or follow commands, may move spontaneously |
| 1 | Unarousable | Minimal or no response to noxious stimuli, does not communicate or follow commands |
| Guidelines for SAS Assessment 1. Agitated patients are scored by their most severe degree of agitation as described 2. If patient is awake or awakens easily to voice (“awaken” means responds with voice or head shaking to a question or follows commands), that’s a SAS 4 (same as calm and appropriate – might even be napping). 3. If more stimuli such as shaking is required but patient eventually does awaken, that’s SAS 3. 4. If patient arouses to stronger physical stimuli (may be noxious) but never awakens to the point of responding yes/no or following commands, that’s a SAS 2. 5. Little or no response to noxious physical stimuli represents a SAS 1. | ||
| This helps separate sedated patients into those you can eventually wake up (SAS 3), those you can't awaken but can arouse (SAS 2), and those you can’t arouse (SAS 1). | ||
Confusion Assessment Method for the ICU (CAM-ICU)
CAM-ICU is a quick way to clinically assess the presence of delirium in an ICU patient. Four different mental recognition features are assessed.
Feature 1: Acute onset or fluctuating course.
Is the patient’s mental status changed compared to the patient’s previous status? Or
Are there signs of a change in mental status in the last 24 hours, as evidenced by fluctuations in the sedation scale (i.e., RASS, MAAS), RLS 85, GCS, or previous delirium assessment.
If no; CAM-ICU negative – no delirium.
If yes: Feature 2. Inattention.
ASE letter test: Tell the patient: “I will now say 10 letters out loud. Every time you hear the letter A, squeeze my hand.” Read the letters SAVEAHAART in a normal tone with 3-second intervals. Incorrect answer: No hand squeeze at the letter A or hand squeeze at other letters. If now 0-2 errors: CAM-ICU negative – no delirium.
More than 2 errors:
Feature 3: Altered level of consciousness.
Occurs if RASS is anything other than 0 or MAAS is anything other than 3. If RASS is anything other than 0: CAM-ICU positive – delirium. MAAS anything other than 3: CAM-ICU positive – delirium.
If RASS=0:
Feature 4: Disorganized thinking.
- Can a stone float in water?
- Are there fish in the sea?
- Does one kilogram weigh more than two kilograms?
- Do you use a hammer to drive in nails?
Instructions (tell the patient)
- “Hold up as many fingers as I do.” (hold up two fingers in front of the patient).
- “Now do the same with the other hand.” (without holding up two fingers).
- If the patient cannot move both arms, instead ask the patient: “Hold up one more finger.”
More than 1 error: CAM-ICU positive – delirium.
0-1 errors: CAM-ICU negative – no delirium.
ICU delirium = Features 1 and 2 occur together with Features 3 or 4.
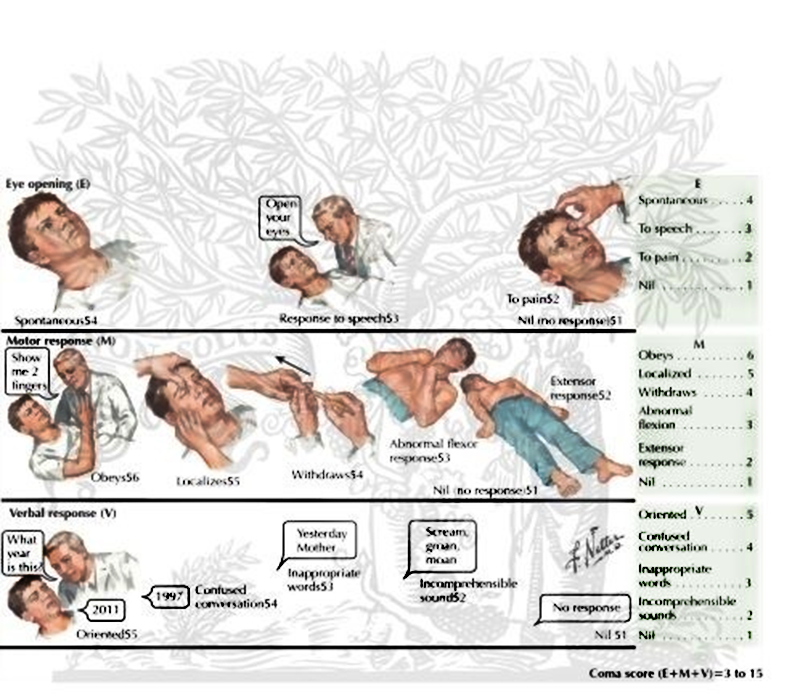
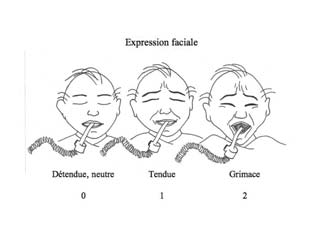
The Critical-Care Pain Observation Tool (CPOT)
| Indicator | Score | Description | Score |
|---|---|---|---|
| Facial expression | Relaxed, neutral | No muscle tension observed | 0 |
| Tense | Presence of frowning, brow lowering, orbit tightening and levator contraction or any other change (e.g. opening eyes or tearing during nociceptive procedures) | 1 | |
| Grimacing | All previous facial movements plus eyelid tightly closed (the patient may present with mouth open or biting the endotracheal tube) | 2 | |
| Body movements | Absence of movements or normal position | Does not move at all (doesn’t necessarily mean absence of pain) or normal position (movements not aimed toward the pain site or not made for the purpose of protection) | 0 |
| Protection | Slow, cautious movements, touching or rubbing the pain site, seeking attention through movements | 1 | |
| Restlessness/Agitation | Pulling tube, attempting to sit up, moving limbs/thrashing, not following commands, striking | 2 | |
| Compliance with the ventilator (intubated patients) | Tolerating ventilator or movement | Alarms not activated, easy ventilation | 0 |
| Coughing but tolerating | Coughing,, alarms may be activated but stop spontaneously | 1 | |
| Fighting ventilator | Asynchrony: blocking ventilation, alarms | 2 | |
| OR | |||
| Vocalization (extubated patients) | Talking in normal tone or no sound | Talking in normal tone or no sound | 0 |
| Sighing, moaning | Sighing, moaning | 1 | |
| Crying out, sobbing | Crying out, sobbing | 2 | |
| Muscle tension | Relaxed | No resistance to passive movements | 0 |
| Evaluation by passive flexion and extension of upper limbs when patient is at rest or evaluation when patient is being turned | Tense, rigid | Resistance to passive movements | 1 |
| Very tense or rigid | Strong resistance to passive movements or incapacity to complete them | 2 | |
| Total | _/8 | (Gélinas et al., 2006) |
Comparison of three of the commonly used sedation scores
| Sedation score by Ready et al. | Pasero opioid-induced sedation scale | Sedation score recommended by ANZCA FPM |
|---|---|---|
| 0 (none) alert | S = Sleep, easily aroused | 0 = wide awake |
| 1 (mild) occasionally drowsy, easy to arouse | 1 = Awake and alert | 1 = easy to rouse (and can stay awake) |
| 2 (moderate) frequently drowsy; easy to arouse | 2 = Occasionally drowsy | 2 = easy to rouse but unable to remainawake |
| 3 (severe) somnolent, difficult to arouse | 3 = Frequently drowsy, arousable, drifts off to sleep difficult to arouse during conversation. | 3 = difficult to rouse Score of 2 = early opioid-inducedventilatory impairment. Titrate opioid so that score is always < 2. |
| S (sleeping) normal sleep, easy to arouse | 4 = Somnolent, minimal or noresponse to stimulation. Subsequently updated, and nowaccompanied by instructions outlining appropriate actions | |
| ANZCA FPM, Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine | ||
National Early Warning Score (NEWS)
NEWS (National Early Warning Score) is used to assess the vital functions of adult patients (≥ 16 years) such as breathing, circulation, and consciousness. NEWS was developed in the UK [1, 2]. It is a validated tool for assessing vital parameters, enabling early identification of critical illness. The vital parameters consist of:
- Respiratory rate
- Oxygen saturation
- Temperature
- Systolic blood pressure
- Heart rate
- Level of consciousness
When comparing different assessment tools for identifying critical illness, NEWS was the best at identifying patients needing intensive care and mortality within 24 hours [3].
Monitoring of vital parameters with NEWS
| Physiological parameters | 3 | 2 | 1 | 0 | 1 | 2 | 3 |
|---|---|---|---|---|---|---|---|
| Respiratory rate | ≤ 8 | 9-11 | 12-20 | 21-24 | ≥ 25 | ||
| Oxygenation | ≤ 91 | 92-93 | 94-95 | ≥ 96 | |||
| Oxygen supply | Ja | Nej | |||||
| Temperature | ≤ 35.0 | 35.1-36.0 | 36.1-38.0 | 38.1-39.0 | ≥ 39.1 | ||
| Systolic blood pressure | ≤ 90 | 91-100 | 101-110 | 111-219 | ≥ 220 | ||
| Heart rate/pulse | ≤ 40 | 41-50 | 51-90 | 91-110 | 111-130 | ≥ 131 | |
| Level of consciousness | A | V, P or U |
NEWS scores should be documented in the data record under a separate heading. NEWS scores >5 should be followed by a comment and action, which is a medical order.
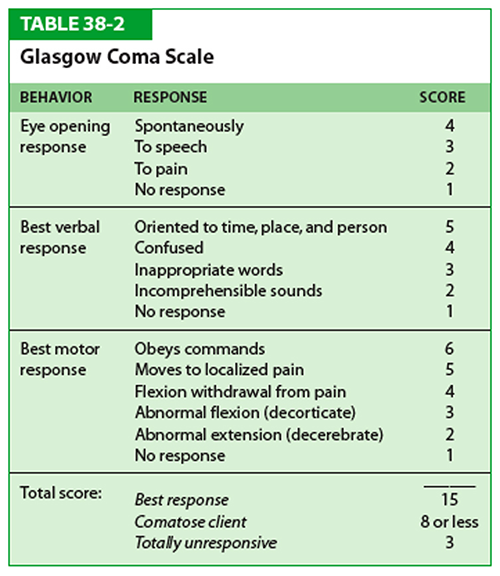
Glasgow Coma Scale (GCS)
A consciousness grading scale that sums up points from three different reactions: eye opening, verbal response, and motor response. A response score below 10 indicates unconsciousness.
Glasgow Coma Scale
| Glasgow Coma Scale | |||||||
|---|---|---|---|---|---|---|---|
| Score: | 1 | 2 | 3 | 4 | 5 | 6 | Score |
| Eye opening | No response | Reaction to pain | To speech | Spontaneously | |||
| Verbal answer | No response | Incomprehensible sounds | Inappropriate words | Confused | Oriented to time, place, person | ||
| Motor answer | No response | Abnormal extension (decerebrate) | Abnormal flexion (decorticated) | Flexion withdrawal from pain | Moves to localized pain | Obeys commands | |
| Sum of Score: | 0-3 p: No response | 3-8: Comatose | 8-14: Stuporous, drowsy | 15: Fully awake | |||
Glasgow Coma Scale
The Glasgow Coma Scale (GCS) is an internationally used scale for assessing the level of consciousness. The scale consists of three tests: eye opening, verbal response, and motor response. Responses are graded with points as shown below. In Sweden, the Swedish model RLS-85 is also used.
Eye Opening
4: Eyes open spontaneously
3: Eyes open to verbal command
2: Eyes open to pain stimulation
1: No eye opening to pain stimulation
Verbal Response
5: Fully oriented
4: Disoriented, confused
3: Responds to speech with single words. Speaks incoherently but understandable words
2: Responds to speech with inarticulate sounds. Unintelligible words, grunts
1: No response to speech
Motor Response
6: Obeys commands adequately
5: Localizes pain
4: Withdrawal movement to pain stimulation. Withdraws arm when pain is stimulated on the fingernail bed
3: Flexion in the elbow to pain stimulation. Stereotypical flexion movement to pain stimulation
2: Extension in the elbow to pain stimulation. Stereotypical extension movement to pain stimulation
1: No response to pain stimulation
Summarize the points:
The maximum score for a fully awake patient is 15 points. A comatose patient receives a minimum of 3 points.
Reaction Level Scale (RLS)
Definitions RLS-85
- RLS 1: Awake. No delayed reaction. Oriented.
- RLS 2: Lethargic or unclear. Contactable with light stimulation such as verbal command, single call, or touch.
- RLS 3: Very lethargic or unclear. Contactable with strong stimulation such as repeated calls, shaking, or pain stimulation. Can, for example, follow with eyes, fixate, obey a command, utter single words, or avert pain stimulation.
………………………… Borderline for unconsciousness ……………………………………………………………….
- RLS 4: Unconscious. Localizes but does not avert pain.
- RLS 5: Unconscious. Withdrawal movement to pain.
- RLS 6: Unconscious. Stereotypical flexion movement to pain (decortication). The wrist, fingers, and elbow flex. The leg extends and rotates inward.
- RLS 7: Unconscious. Stereotypical extension movement to pain (decerebration). Opisthotonus, extension of the neck, clenched jaws, pronated, adducted, extended arms, and legs.
- RLS 8: Unconscious. No pain reaction.
Awake: Not lethargic, fully oriented. Intubated patient: No signs of delayed reaction.
Lethargic: The patient is lethargic if he/she feels or cooperates poorly and responds or reacts with a delayed reaction.
Unclear: If the patient answers incorrectly to any of the following three questions, he is unclear: a/ “What is your name?” (first and last name). b/ “Where are you?” (location, e.g., city name or “in hospital”). c/ “What year and month is it now?”.
Contactable: Can be awakened. The patient can perform one of the following: Engage in conversation or utter words – follow with eyes – obey command – avert pain.
Follow with eyes: Eye opening with eye contact and at some point a clear attempt to follow with the eyes.
Obey command: Upon command, the patient performs a specific movement, e.g., “raise your arms,” “stick out your tongue,” or “close your eyes.”
Avert pain: The patient localizes the pain stimulus, actively grips, and tries to remove it.
Unconscious: Cannot be awakened. Cannot perform any of the tasks required for contactability.
Localize pain: The patient is examined lying on his back with arms resting on the surface alongside the body. a/ When stimulated in the jaw angle, the patient moves a hand above chin level, or b/ when stimulated against the nail bed of one hand, the patient moves the other hand across the midline.
Withdrawal movement: a/ When stimulated in the jaw angle, the patient turns away the face, or b/ when stimulated against the nail bed, the patient does not localize the pain but clearly withdraws the arm from the trunk.
Stereotypical flexion movement: Upon pain stimulation, the patient slowly and mechanically bends the elbow and wrist but cannot localize or withdraw.
Stereotypical extension movement: Upon pain stimulation, the patient extends the arms or legs. If both flexion and extension movements occur, the flexion movement is noted, i.e., the best response applies.
No pain reaction: The patient does not move arms or legs or grimace at pain stimulation.

Glasgow Coma Scale Children

Focal Neurology
Neurological Parameters
Score Estimation
Total Score
1a. Level of Consciousness
According to RLS-85.
- 0 = Alert and awake (RLS 1).
- 1 = Lethargic but responsive to light stimulation (RLS 2).
- 2 = Very lethargic, requires repeated or painful stimuli for response or to follow commands (RLS 3).
- 3 = Coma. Patient unresponsive. Reflex or automatic movements (RLS 4–8).
1b. Orientation
Ask the patient about the current month and the patient’s age.
Do not give any hints. The first answer counts.
- 0 = Two correct.
- 1 = One correct. Also given if intubated/dysarthria/other speech difficulty.
- 2 = None correct. Given if aphasia/coma.
1c. Comprehension
Give commands (without showing). Close your eyes!
Clench your hand! (non-paretic side).
If the patient is aphasic, pantomime is used.
- 0 = Two correct.
- 1 = One correct.
- 2 = None correct.
- Eye Movement/Positioning
First observe eye position, then test eye movements to the right and left. If the patient does not follow the commands, try the doll’s eye maneuver (turn the head).
- 0 = Normal.
- 1 = Partial gaze palsy (deviation conjugée) which can be overcome voluntarily or with doll’s eye maneuver. Partial eye muscle paresis.
- 2 = Complete gaze palsy (deviation conjugée) which cannot be overcome voluntarily or with doll’s eye maneuver.
- Visual Field
Use the confrontation test, e.g., finger counting or by moving the hand “threateningly” towards the patient’s eye. If the patient is blind in one eye, check the healthy eye.
- 0 = Normal.
- 1 = Partial hemianopia (e.g., quadrantanopia). If visual neglect is present (tested with bimanual confrontation), record 1 point under item 11.
- 2 = Complete hemianopia.
- 3 = Bilateral visual field defects (e.g., blindness including cortical blindness).
- Facial Palsy
Ask the patient to show teeth, raise eyebrows, and close eyes. In a lethargic or aphasic patient, assess the reaction to painful stimuli.
- 0 = Normal.
- 1 = Partial central facial palsy (flattened nasolabial fold, asymmetry when smiling).
- 2 = Complete central facial palsy (total or almost total paralysis of the lower half of the face).
- 3 = Peripheral facial palsy (upper and lower half of the face). Bilateral facial palsy.
- Arm Paresis
Stretch the arm 45 degrees if lying or 90 degrees if sitting. Ask the patient to hold for 10 seconds. Test the non-paretic side first. Amputation or contracture gives 0 points.
- 0 = Holds for 10 seconds.
- 1 = Sinks but does not reach the bed within < 10 seconds.
- 2 = Falls to the bed within < 10 seconds. Some resistance to gravity.
- 3 = The arm falls immediately but can move toward the bed.
- 4 = No movement in the arm.
Right:
Left:
- Leg Paresis
The patient is lying down. Raise the leg to 30 degrees. Ask the patient to hold for 5 seconds. Test the non-paretic side first. Amputation or contracture gives 0 points.
- 0 = Holds for 5 seconds.
- 1 = Sinks but does not reach the bed within < 5 seconds.
- 2 = Falls to the bed within < 5 seconds. Some resistance to gravity.
- 3 = The leg falls immediately but can move toward the bed.
- 4 = No movement in the leg.
Right:
Left:
- Ataxia
Tested with heel-to-knee and finger-to-nose tests. Refers only to cerebellar symptoms (open eyes). If the patient is amputated, does not understand, or is hemiparetic, 0 points are given.
- 0 = Normal.
- 1 = Ataxia in one extremity.
- 2 = Ataxia in two extremities.
- Sensation (Pain)
Tested with a needle. Refers only to dysfunction due to stroke. In a lethargic or aphasic patient, assess with painful stimuli. A patient in a coma is given 2 points.
- 0 = Normal.
- 1 = Mild to moderate reduction, varying degrees of altered sensory perception, but the patient is aware of being touched.
- 2 = Severe or total reduction, the patient is unaware of being touched. Patient with brainstem stroke and bilateral sensory reduction. Patient in a coma.
- Speech/Communication
Ask the patient to describe the picture, name the objects, and read the sentences.
- 0 = Normal.
- 1 = Mild to moderate dysphasia. Difficulty naming and finding words, paraphrasia, circumlocutions, or mild to moderate difficulty understanding or expressing.
- 2 = Severe aphasia.
- 3 = Mute or global aphasia, no usable speech or comprehension.
- Dysarthria
Ask the patient to read words from the list, do not explain why! Intubated patients are given 0 points.
- 0 = Normal.
- 1 = Mild dysarthria, slurs a few words or understandable with difficulty.
- 2 = Severe dysarthria, speech is incomprehensible or the patient is mute.
- Extinction/Neglect
A. Based on previous tests, especially visual fields and language.
B. Ask the patient to close their eyes. Touch both the right and left sides simultaneously. If there is a pronounced visual field defect but normal perception of skin stimulation, 0 points are given. If the patient has aphasia, 0 points are also given if they appear to respond normally to skin stimulation.
- 0 = Normal.
- 1 = One modality reduced (i.e., visual or tactile neglect in bilateral simultaneous stimulation).
- 2 = Pronounced unilateral neglect. Inattention to both visual and tactile stimulation. Does not recognize their own hand.
NIH Stroke Scale
| Neurological Parameters | Score Estimation | Total Score | |
|---|---|---|---|
| 1a. Level of Consciousness According to RLS-85. | 0 = Alert and awake (RLS 1). 1 = Lethargic but responsive to light stimulation (RLS 2). 2 = Very lethargic, requires repeated or painful stimuli for response or to follow commands (RLS 3). 3 = Coma. Patient unresponsive. Reflex or automatic movements (RLS 4–8). | ||
| 1b. Orientation Ask the patient about the current month and the patient’s age. Do not give any hints. The first answer counts. | 0 = Two correct. 1 = One correct. Also given if intubated/dysarthria/other speech difficulty. 2 = None correct. Given if aphasia/coma. | ||
| 1c. Comprehension Give commands (without showing). Close your eyes! Clench your hand! (non-paretic side). If the patient is aphasic, pantomime is used. | 0 = Two correct. 1 = One correct. 2 = None correct. | ||
| 2. Eye Movement/Positioning First observe eye position, then test eye movements to the right and left. If the patient does not follow the commands, try the doll’s eye maneuver (turn the head). | 0 = Normal. 1 = Partial gaze palsy (deviation conjugée) which can be overcome voluntarily or with doll’s eye maneuver. Partial eye muscle paresis. 2 = Complete gaze palsy (deviation conjugée) which cannot be overcome voluntarily or with doll’s eye maneuver. | ||
| 3. Visual Field Use the confrontation test, e.g., finger counting or by moving the hand "threateningly" towards the patient’s eye. If the patient is blind in one eye, check the healthy eye. | 0 = Normal. 1 = Partial hemianopia (e.g., quadrantanopia). If visual neglect is present (tested with bimanual confrontation), record 1 point under item 11. 2 = Complete hemianopia. 3 = Bilateral visual field defects (e.g., blindness including cortical blindness). | ||
| 4. Facial Palsy Ask the patient to show teeth, raise eyebrows, and close eyes. In a lethargic or aphasic patient, assess the reaction to painful stimuli. | 1 = Partial central facial palsy (flattened nasolabial fold, asymmetry when smiling). 2 = Complete central facial palsy (total or almost total paralysis of the lower half of the face). 3 = Peripheral facial palsy (upper and lower half of the face). Bilateral facial palsy. | ||
| 5. Arm Paresis Stretch the arm 45 degrees if lying or 90 degrees if sitting. Ask the patient to hold for 10 seconds. Test the non-paretic side first. Amputation or contracture gives 0 points. | 0 = Holds for 10 seconds. 1 = Sinks but does not reach the bed within < 10 seconds. 2 = Falls to the bed within < 10 seconds. Some resistance to gravity. 3 = The arm falls immediately but can move toward the bed. 4 = No movement in the arm. | Right:_ Left:_ | |
| 6. Leg Paresis The patient is lying down. Raise the leg to 30 degrees. Ask the patient to hold for 5 seconds. Test the non-paretic side first. Amputation or contracture gives 0 points. | 0 = Holds for 5 seconds. 1 = Sinks but does not reach the bed within < 5 seconds. 2 = Falls to the bed within < 5 seconds. Some resistance to gravity. 3 = The leg falls immediately but can move toward the bed. 4 = No movement in the leg. | Right:_ Left:_ | |
| 7. Ataxia Tested with heel-to-knee and finger-to-nose tests. Refers only to cerebellar symptoms (open eyes). If the patient is amputated, does not understand, or is hemiparetic, 0 points are given. | 0 = Normal. 1 = Ataxia in one extremity. 2 = Ataxia in two extremities | ||
| 8. Sensation (Pain) Tested with a needle. Refers only to dysfunction due to stroke. In a lethargic or aphasic patient, assess with painful stimuli. A patient in a coma is given 2 points. | 0 = Normal. 1 = Mild to moderate reduction, varying degrees of altered sensory perception, but the patient is aware of being touched. 2 = Severe or total reduction, the patient is unaware of being touched. Patient with brainstem stroke and bilateral sensory reduction. Patient in a coma. | ||
| 9. Speech/Communication Ask the patient to describe the picture, name the objects, and read the sentences. | 0 = Normal. 1 = Mild to moderate dysphasia. Difficulty naming and finding words, paraphrasia, circumlocutions, or mild to moderate difficulty understanding or expressing. 2 = Severe aphasia. 3 = Mute or global aphasia, no usable speech or comprehension. | ||
| 10. Dysarthria Ask the patient to read words from the list, do not explain why! Intubated patients are given 0 points. | 0 = Normal. 1 = Mild dysarthria, slurs a few words or understandable with difficulty. 2 = Severe dysarthria, speech is incomprehensible or the patient is mute. | ||
| 11. Extinction/Neglect A. Based on previous tests, especially visual fields and language. B. Ask the patient to close their eyes. Touch both the right and left sides simultaneously. If there is a pronounced visual field defect but normal perception of skin stimulation, 0 points are given. If the patient has aphasia, 0 points are also given if they appear to respond normally to skin stimulation. | 0 = Normal. 1 = One modality reduced (i.e., visual or tactile neglect in bilateral simultaneous stimulation). 2 = Pronounced unilateral neglect. Inattention to both visual and tactile stimulation. Does not recognize their own hand. |
Muscle Strength Grading-Scale (MSG-Scale)
| The strength of the extremities is assessed using the Muscle Strength Grading-scale (MSG-Scale) where five is normal strength and zero is paralysis | ||
|---|---|---|
| 0 | No contraction | Paralysis |
| 1 | Flicker of contraction | Visible or palpable contraction |
| 2 | Active movement; can’t resist gravity | Moves but not against gravity (i.e. does not lift off the surface) |
| 3 | Active movement against gravity | Move against gravity (i.e. lift off the ground) |
| 4 | Active movement against resistance | Move against gravity and actively against resistance |
| 5 | Normal strength | Normal strength |
NIH Stroke Scale
NIH Stroke Scale
| Neurological Parameters | Score Estimation | Total Score | |
|---|---|---|---|
| 1a. Level of Consciousness According to RLS-85. | 0 = Alert and awake (RLS 1). 1 = Lethargic but responsive to light stimulation (RLS 2). 2 = Very lethargic, requires repeated or painful stimuli for response or to follow commands (RLS 3). 3 = Coma. Patient unresponsive. Reflex or automatic movements (RLS 4–8). | ||
| 1b. Orientation Ask the patient about the current month and the patient’s age. Do not give any hints. The first answer counts. | 0 = Two correct. 1 = One correct. Also given if intubated/dysarthria/other speech difficulty. 2 = None correct. Given if aphasia/coma. | ||
| 1c. Comprehension Give commands (without showing). Close your eyes! Clench your hand! (non-paretic side). If the patient is aphasic, pantomime is used. | 0 = Two correct. 1 = One correct. 2 = None correct. | ||
| 2. Eye Movement/Positioning First observe eye position, then test eye movements to the right and left. If the patient does not follow the commands, try the doll’s eye maneuver (turn the head). | 0 = Normal. 1 = Partial gaze palsy (deviation conjugée) which can be overcome voluntarily or with doll’s eye maneuver. Partial eye muscle paresis. 2 = Complete gaze palsy (deviation conjugée) which cannot be overcome voluntarily or with doll’s eye maneuver. | ||
| 3. Visual Field Use the confrontation test, e.g., finger counting or by moving the hand "threateningly" towards the patient’s eye. If the patient is blind in one eye, check the healthy eye. | 0 = Normal. 1 = Partial hemianopia (e.g., quadrantanopia). If visual neglect is present (tested with bimanual confrontation), record 1 point under item 11. 2 = Complete hemianopia. 3 = Bilateral visual field defects (e.g., blindness including cortical blindness). | ||
| 4. Facial Palsy Ask the patient to show teeth, raise eyebrows, and close eyes. In a lethargic or aphasic patient, assess the reaction to painful stimuli. | 1 = Partial central facial palsy (flattened nasolabial fold, asymmetry when smiling). 2 = Complete central facial palsy (total or almost total paralysis of the lower half of the face). 3 = Peripheral facial palsy (upper and lower half of the face). Bilateral facial palsy. | ||
| 5. Arm Paresis Stretch the arm 45 degrees if lying or 90 degrees if sitting. Ask the patient to hold for 10 seconds. Test the non-paretic side first. Amputation or contracture gives 0 points. | 0 = Holds for 10 seconds. 1 = Sinks but does not reach the bed within < 10 seconds. 2 = Falls to the bed within < 10 seconds. Some resistance to gravity. 3 = The arm falls immediately but can move toward the bed. 4 = No movement in the arm. | Right:_ Left:_ | |
| 6. Leg Paresis The patient is lying down. Raise the leg to 30 degrees. Ask the patient to hold for 5 seconds. Test the non-paretic side first. Amputation or contracture gives 0 points. | 0 = Holds for 5 seconds. 1 = Sinks but does not reach the bed within < 5 seconds. 2 = Falls to the bed within < 5 seconds. Some resistance to gravity. 3 = The leg falls immediately but can move toward the bed. 4 = No movement in the leg. | Right:_ Left:_ | |
| 7. Ataxia Tested with heel-to-knee and finger-to-nose tests. Refers only to cerebellar symptoms (open eyes). If the patient is amputated, does not understand, or is hemiparetic, 0 points are given. | 0 = Normal. 1 = Ataxia in one extremity. 2 = Ataxia in two extremities | ||
| 8. Sensation (Pain) Tested with a needle. Refers only to dysfunction due to stroke. In a lethargic or aphasic patient, assess with painful stimuli. A patient in a coma is given 2 points. | 0 = Normal. 1 = Mild to moderate reduction, varying degrees of altered sensory perception, but the patient is aware of being touched. 2 = Severe or total reduction, the patient is unaware of being touched. Patient with brainstem stroke and bilateral sensory reduction. Patient in a coma. | ||
| 9. Speech/Communication Ask the patient to describe the picture, name the objects, and read the sentences. | 0 = Normal. 1 = Mild to moderate dysphasia. Difficulty naming and finding words, paraphrasia, circumlocutions, or mild to moderate difficulty understanding or expressing. 2 = Severe aphasia. 3 = Mute or global aphasia, no usable speech or comprehension. | ||
| 10. Dysarthria Ask the patient to read words from the list, do not explain why! Intubated patients are given 0 points. | 0 = Normal. 1 = Mild dysarthria, slurs a few words or understandable with difficulty. 2 = Severe dysarthria, speech is incomprehensible or the patient is mute. | ||
| 11. Extinction/Neglect A. Based on previous tests, especially visual fields and language. B. Ask the patient to close their eyes. Touch both the right and left sides simultaneously. If there is a pronounced visual field defect but normal perception of skin stimulation, 0 points are given. If the patient has aphasia, 0 points are also given if they appear to respond normally to skin stimulation. | 0 = Normal. 1 = One modality reduced (i.e., visual or tactile neglect in bilateral simultaneous stimulation). 2 = Pronounced unilateral neglect. Inattention to both visual and tactile stimulation. Does not recognize their own hand. |
Glasgow Outcome Scale
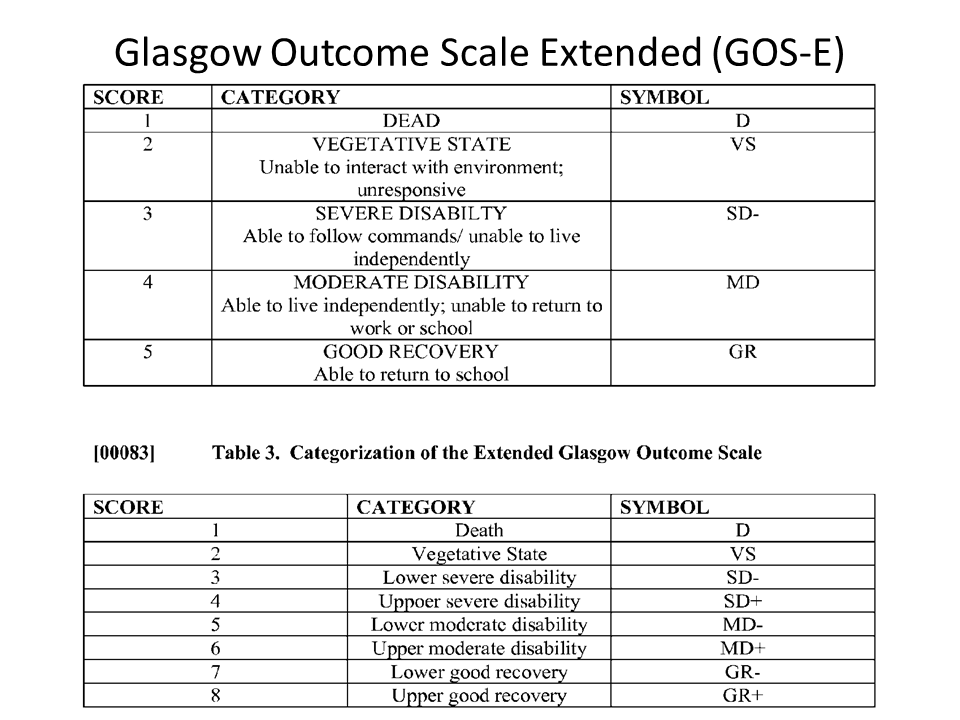
The Glasgow Outcome Scale (GOS) is a global scale for functional outcomes that categorizes the patient’s status into one of five categories: death, vegetative state, severe disability, moderate disability, or good recovery. The extended GOS (GOSE) provides more detailed categorization into eight categories by splitting the categories of severe disability, moderate disability, and good recovery into lower and upper categories:
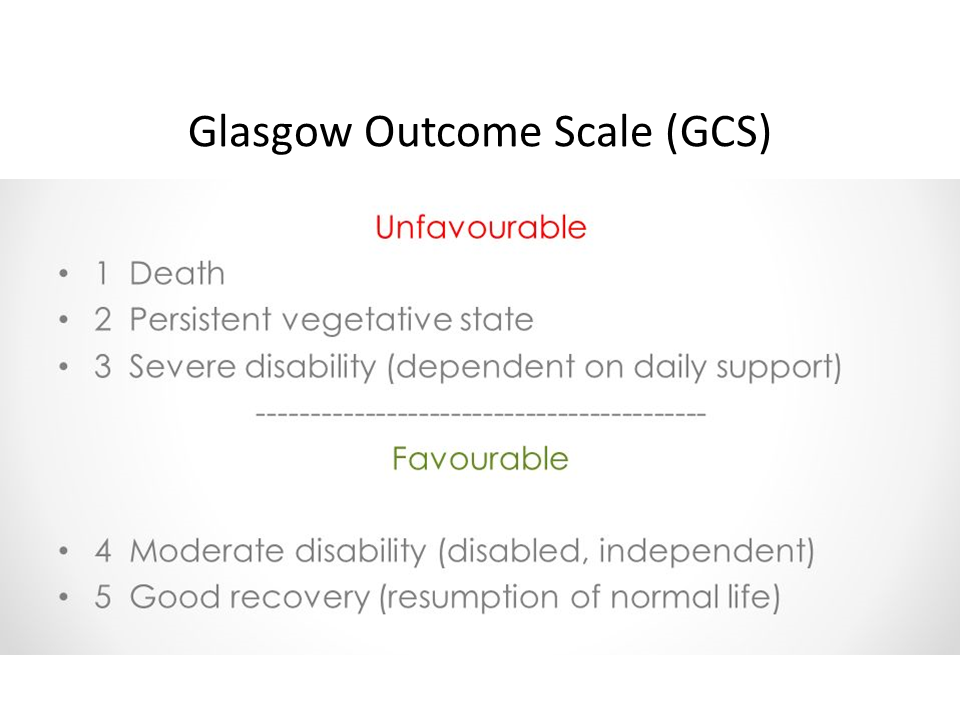
Glasgow Outcome Scale
| Degree | Outcome | |
|---|---|---|
| 1 | Death | Severe injury or death without recovery of consciousness |
| 2 | Persistent vegetative state | Severe damage with prolonged state of unresponsiveness and a lack of higher mental functions |
| 3 | Severe disability | Severe injury with permanent need for help with daily living |
| 4 | Moderate disability | No need for assistance in everyday life, employment is possible but may require special equipment. |
| 5 | Low disability | Light damage with minor neurological and psychological deficits. |
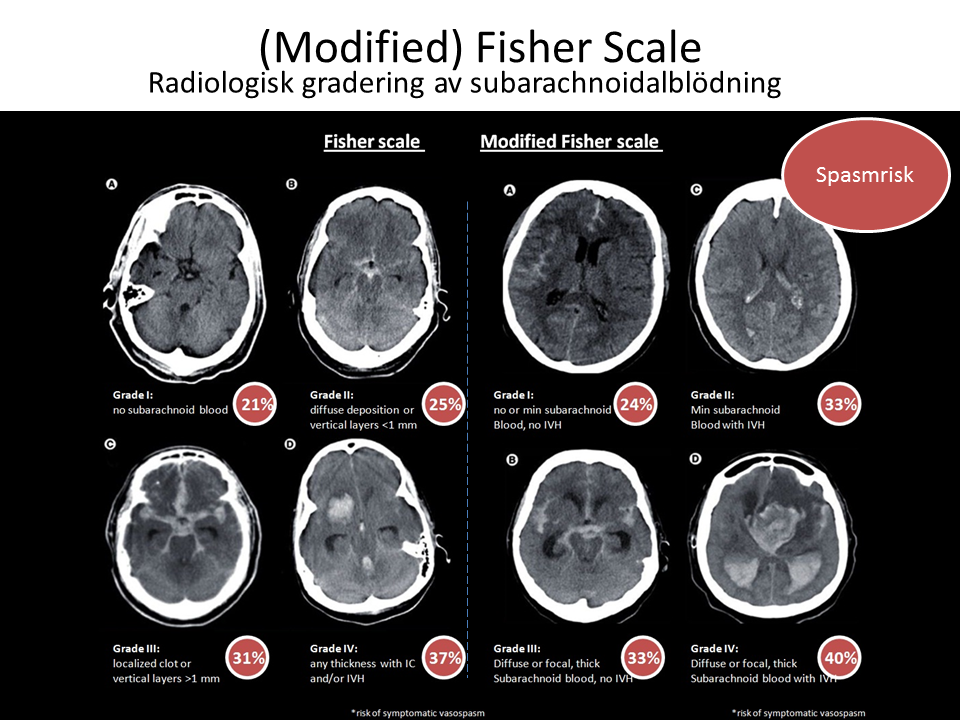
Fisher Scale (modified) – SAH
| Score | Degree of subarachnoid haemorrhage |
|---|---|
| Grade 1 | No subarachnoid (SAH) or intraventricular haemorrhage (IVH) detected |
| | Incidence of symptomatic vasospasm: 21% |
| Grade 2 | Diffuse thin (<1 mm) SAH |
| No clots | |
| Incidence of symptomatic vasospasm: 25% | |
| Grade 3 | Localised clots and/or layers of blood >1 mm in thickness |
| No IVH | |
| Incidence of symptomatic vasospasm: 37% | |
| Grade 4 | Diffuse or no SAH |
| ICH or IVH present | |
| Incidence of symptomatic vasospasm: 31% |
Hunt & Hess / WFNS grading
Clinical grading of a subarachnoid hemorrhage.
The Hunt and Hess scale describes the severity of subarachnoid hemorrhage and is used as a predictor of survival.
The Hunt & Hess Scale
| Grade 1 | Asymptomatic or minimal headache and slight neck stiffness | 70% survival |
|---|---|---|
| Grade 2 | Moderate to severe headache; neck stiffness; no neurologic deficit except cranial nerve palsy | 60% survival |
| Grade 3 | Drowsy; minimal neurologic deficit | 50% survival |
| Grade 4 | Stuporous; moderate to severe hemiparesis; possibly early decerebrate rigidity and vegetative disturbances | 20% survival |
| Grade 5 | Deep coma; decerebrate rigidity; moribund | 10% survival |
Hunt & Hess Classification of Subarachnoid Hemorrhage
| Clinical picture | Class |
|---|---|
| Mild Headache, Alert and Oriented, Minimal (if any) Nuchal Rigidity | +1 |
| Full Nuchal Rigidity, Moderate-Severe Headache, Alert and Oriented, No Neuro Deficit (Besides CN Palsy) | +2 |
| Lethargy or Confusion, Mild Focal Neurological Deficits | +3 |
| Stuporous, More Severe Focal Deficit | +4 |
| Comatose, showing signs of severe neurological impairment (ex: posturing) | +5 |
CPC – Cerebral Performance Categories
| Outcome of Brain Injury: | The Glasgow-Pittsburgh Cerebral Performance Scale | Overall Performance Categories | |
|---|---|---|---|
| 1 | Good cerebral performance | Conscious. Alert, able to work and lead a normal life. May have minor psychological or neurological deficits (mild dysphasia, nonincapacitating hemiparesis, or minor cranial nerve abnormalities). | Good overall performance. Healthy, alert, capable of normal life. Good cerebral performance (CPC 1) plus no or only mild functional disability from noncerebral organ system abnormalities. |
| 2 | Moderate cerebral disability | Conscious. Sufficient cerebral function for part-time work in sheltered environment or independent activities of daily life (dressing, traveling by public transportation, and preparing food). May have hemiplegia, seizures, ataxia, dysarthria, dysphasia or permanent memory or mental changes. | Moderate overall disability. Conscious. Moderate cerebral disability alone (CPC 2) or moderate disability from noncerebral system dysfunction alone or both. Performs independent activities of daily life (dressing, traveling, and food preparation). May be able to work part-time in sheltered environment but disabled for competitive work. |
| 3 | Severe cerebral disability | Conscious. Dependent on others for daily support because of impaired brain function (in an institution or at home with exceptional family effort). At least limited cognition. Includes a wide range of cerebral abnormalities from ambulatory with severe memory disturbance or dementia precluding independent existence to paralytic and able to communicate only with eyes, as in the locked-in syndrome. | Several overall disability. Conscious. Severe cerebral disability alone (CPC 3) or severe disability from noncerebral organ system dysfunction alone or both. Dependent on others for daily support. |
| 4 | Coma, vegetative state | Not conscious. Unaware of surroundings, no cognition. No verbal or psychological interactions with environment. | Same as CPC 4 |
| 5 | Death | Certified brain dead or dead by traditional criteria. | Same as CPC 5. |
West Haven Scale for Grading Hepatic Encephalopathy
| Degree of encephalopathy | Clinical picture |
|---|---|
| MINIMAL HEPATIC ENCEPHALOPATHY: | Abnormal test findings but no clinically noticeable changes |
| WEST HAVEN GRADE I: | Cognitive or behavioral disturbance compared to normal state, according to patient, relatives or examiner |
| WEST HAVEN GRADE II: | Obvious personality change, impaired attention, disorientation regarding time, dyspraxia |
| WEST HAVEN GRADE III: | Drowsiness, apparent confusion, disorientation regarding time and place, bizarre behavior |
| WEST HAVEN GRADE IV: | Coma |
Disclaimer:
The content on AnesthGuide.com is intended for use by medical professionals and is based on practices and guidelines within the Swedish healthcare context.
While all articles are reviewed by experienced professionals, the information provided may not be error-free or universally applicable.
Users are advised to always apply their professional judgment and consult relevant local guidelines.
By using this site, you agree to our Terms of Use.