Author:
Kai Knudsen
Updated:
3 December, 2025
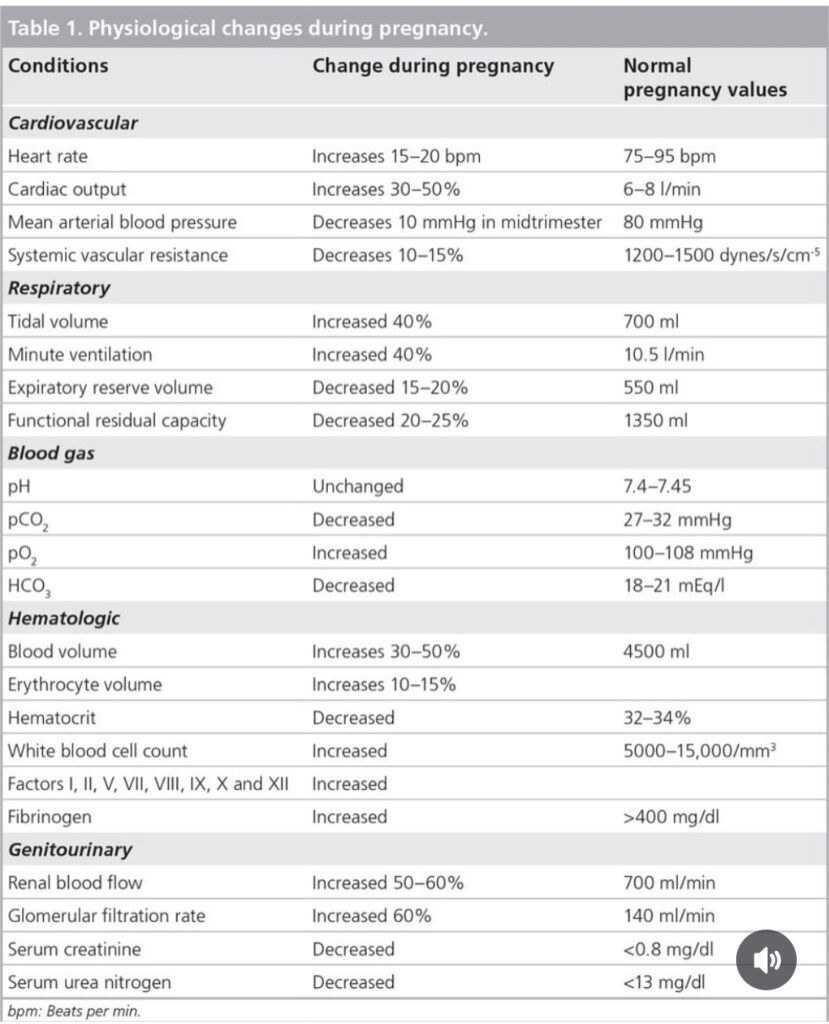
This chapter briefly describes obstetric anesthesia, including epidural anesthesia for labor and spinal or general anesthesia for emergency cesarean section. It includes various drug combinations commonly used for labor epidurals and spinal anesthesia.
- Classification of Urgency for Caesarean Section
- Labor Epidural (EA/EPi)
- PCEA (Continuous EA + PCEA)
- Labor EA with PCEA
- TOP-UP Labor Epidural Before Surgery
- Failing labor epidural
- Obstetric Anesthesia Pocket Guide
- General Anesthesia for Emergency C-Section and Elective C-Section
- Obstetric Spinal Anesthesia
- Severe Postpartum Hemorrhage
- Thiopenthone (Pentocur/Pentothal)
Classification of Urgency for Caesarean Section
Category 1 – Immediate (Crash C-section / Emergency call)
Immediate threat to the life of the baby and/or the mother.
Category 2 – Urgent Caesarean Section
Threat to the life of the baby or the mother. The baby should be delivered within 20–30 minutes.
Category 3 – Non-urgent Caesarean Section
No immediate threat to the life of the baby or the mother.
Category 4 – Elective Caesarean Section
Planned procedure in the regular operating schedule. Regional anesthesia is recommended as first choice.
Aortocaval compression must always be avoided by using a left-tilted operating table or wedge of at least 15 degrees, regardless of the type of anesthesia.
Labor Epidural (EA/EPi)
Indications
- Severe labor pain
- Cesarean section with epidural anesthesia
Contraindications
- Local skin infection
- Coagulation disorder
- Hypovolemia
Technique
The placement of an EPi is preferably done with the patient sitting up, which generally provides better conditions for a smooth and successful placement compared to keeping the patient lying down. A good patient position is essential for successful EPi placement.



Sampling Routines
- Mild preeclampsia, tests no older than 6 hours – Platelet count (PLT)
- Severe preeclampsia, tests < 2 hours old – Platelet count, INR, a-PTT
- IUFD, tests < 4 hours old – Platelet count, INR, a-PTT
Medication, Dosage, and Pump
- Various EA mixtures are used, e.g., Levobupivacaine (Chirocaine) 0.625 mg/ml + Sufentanil 0.5 μg/ml or Bupivacaine 0.6 mg/ml + Sufentanil 0.5 μg/ml 100 ml
- Initial bolus dose administered manually by anesthesiologist: 6 + 6 ml.
- 12 ml is drawn from the medication bag from the area with the syringe symbol. The bag is non-sterile.
Labor Epidural (EPi for Labor Analgesia/EA)
| Drug (Brand name) | Local anesthetics | Opioid | Starting dose | Bolus | Continuous infusion |
|---|---|---|---|---|---|
| Chirocaine 0,0625% + Sufenta 0,05% | Levobupivacaine 0,625 mg/ml | Sufentanil 0,5 μg/ml | 12 ml | 4-8 ml | 8 ml/hour |
| Narop 0,1% + Sufenta 0,1% | Ropivacaine 1 mg/ml | Sufentanil 1 μg/ml | 10 ml | 4-8 ml | 6-9 ml/hour |
| Marcain 0,1% + Sufenta 0,1% | Bupivacaine 1 mg/ml | Sufentanil 1 μg/ml | 10 ml | 4-8 ml | 6-9 ml/hour |
| Narop 0,2% | Ropivacaine 2 mg/ml | 8 ml | 4-8 ml | 2-5 ml/hour | |
| Local anesthetics | Opioid | Starting dose | Bolus | Lockout Time in Pump | |
| Chirocain 0,0625% + Sufenta 0,05% | Levobupivacaine 0,625 mg/ml | Sufentanil 0,5 μg/ml | 12 ml | 4 ml | 15 min |
| Marcaine 0.6 mg/ml + Sufenta 0.5 μg/ml, continuous infusion of 5 ml/hour. | Bupivacaine 0,6 mg/ml | Sufentanil 0,5 μg/ml | 10 ml | 5 ml | Lockout Time in Pump 30 min |

PCEA (Continuous EA + PCEA)
- Continuous EPi 5 ml/hour +
- Patient-administered bolus dose of 5 ml
- Lockout time set to 30 minutes
Continuous EA:
› 8 ml/hour
Midwife-Administered Loading Dose:
› Loading dose 5 ml, 1 time/hour.
Labor EA with PCEA
- Bupivacaine (Marcaine) 0.6 mg/ml + Sufentanil 0.5 μg/ml, continuous infusion of 5 ml/hour, bolus 5 ml. Lockout time 30 minutes.
- Levobupivacaine (Chirocaine) 0.0625% + Sufentanil 0.05%, Start dose 12 ml, bolus 4 ml, lockout time 15 min.
When treating patients in the postoperative/ICU/labor ward, note and document the number of requested bolus doses, the number of delivered doses, and the total dose given. The goal with PCEA is VAS < 4 and 1-2 bolus doses per hour. On the ward, it is important to monitor and check every four hours for VAS, respiratory rate, sedation level, nausea, itching, and bladder function. Extra checks must be done if doses are increased, with checks every 30 minutes for two hours. In case of inadequate pain relief, loading doses can be given every 10 minutes until good pain relief is achieved. If the number of PCEA doses exceeds 3 per hour, the continuous infusion is increased. If inadequate pain relief is achieved at the maximum dose, consider adjunct pain treatment or replacing the epidural.
When treating patients with mild preeclampsia, coagulation tests should be checked no more than 6 hours before placing an EPi. For severe eclampsia, these tests (PT/a-PTT/PLT/Platelet count) should be no more than 2 hours old.
TOP-UP Labor Epidural Before Surgery
EMERGENCY C-SECTION
- Ropivacaine (Naropin) 7.5 mg/ml, 15-20 ml plus
- Sufentanil 5 μg/ml, 2-4 ml = 10-20 μg or
- Fentanyl 50 μg/ml, 1-2 ml = 50-100 μg epidurally
- Special Morphine 0.4 mg/ml, 5 ml = 2 mg (given postpartum – caution with high distribution)
PLACENTAL DETACHMENT / SUTURING BIRTH INJURY
- Sufentanil 5 μg/ml, 2-4 ml = 10-20 μg
- Ropivacaine (Naropin) 7.5 mg/ml, approx. 10 ml
Failing labor epidural


Labor Epidural (EPi for Labor Analgesia/EA)
| Drug (Brand name) | Local anesthetics | Opioid | Starting dose | Bolus | Continuous infusion |
|---|---|---|---|---|---|
| Chirocaine 0,0625% + Sufenta 0,05% | Levobupivacaine 0,625 mg/ml | Sufentanil 0,5 μg/ml | 12 ml | 4-8 ml | 8 ml/hour |
| Narop 0,1% + Sufenta 0,1% | Ropivacaine 1 mg/ml | Sufentanil 1 μg/ml | 10 ml | 4-8 ml | 6-9 ml/hour |
| Marcain 0,1% + Sufenta 0,1% | Bupivacaine 1 mg/ml | Sufentanil 1 μg/ml | 10 ml | 4-8 ml | 6-9 ml/hour |
| Narop 0,2% | Ropivacaine 2 mg/ml | 8 ml | 4-8 ml | 2-5 ml/hour | |
| Local anesthetics | Opioid | Starting dose | Bolus | Lockout Time in Pump | |
| Chirocain 0,0625% + Sufenta 0,05% | Levobupivacaine 0,625 mg/ml | Sufentanil 0,5 μg/ml | 12 ml | 4 ml | 15 min |
| Marcaine 0.6 mg/ml + Sufenta 0.5 μg/ml, continuous infusion of 5 ml/hour. | Bupivacaine 0,6 mg/ml | Sufentanil 0,5 μg/ml | 10 ml | 5 ml | Lockout Time in Pump 30 min |
Conversion of Labor Epidural to C-Section Epidural ("Top-Up")
| Local anesthetics | Brand name | Strength | Volume (ml) | Dose (mg) | Opioid |
|---|---|---|---|---|---|
| Ropivacaine | Naropine® | 5 mg/ml | 15-20 ml | 113-150 mg | + Sufentanil 25 μg |
| Levobupivacaine | Chirocain®* | 5 mg/ml | 15–20 ml | 75–100 mg | |
| Bupivacaine | Marcaine® | 5 mg/ml, | 15–20 ml | 75–100 mg | |
| Chlorprocaine | Nesacaine ® | 30 mg/ml (3% ) | 15–20 ml | ||
| * slow injection | |||||
Epidural anesthesia for caesarean section (sectio)
| Local anesthetics | Brand name | Strength | Volume (ml) | Dose (mg) |
|---|---|---|---|---|
| Levobupivacaine | Chirocaine® | 5 mg/ml* | 15–30 ml | 75–150 mg |
| Mepivacaine | Carbocaine® | 20 mg/ml | 10–17,5 ml | 200–350 mg |
| Bupivacaine | Marcaine® | 5 mg/ml | 15–30 ml | 75–150 mg |
| Chloroprocaine | Nesacaine®3% | 30 mg/ml | 15–20 ml i bolus | |
| Ropivacaine | Naropine® | 7,5 mg/ml | 15-20 ml | 112,5-150 mg |
| * slow administration | ||||
Spinal Anesthesia for Cesarean Sectio
| Drug (Brand name) | Local anesthetics | Concentration | Dose (ml) | Opioid |
|---|---|---|---|---|
| Marcaine Spinal Heavy | Bupivacaine with Glucose | 5 mg/ml | 1,8–2,4 ml (7,5–12,5 mg) | |
| Marcaine Spinal Heavy | Bupivacaine with Glucose | 5 mg/ml | 1,8-2,4 ml + | Fentanyl 15-25 μg |
| Marcaine Spinal Heavy | Bupivacaine with Glucose | 5 mg/ml | 1,8-2,4 ml + | Morphine 0,1 mg (0.4 mg/ml 0.25 ml) |
| Marcaine Spinal Heavy | Bupivacaine with Glucose | 5 mg/ml | 1,8-2,4 ml + | Fentanyl 15-25 μgram + Morphine 0,1 mg (0,4 mg/ml 0,25 ml) |
| Naropin | Ropivacaine | 5 mg/ml | 1,5-3 ml (7,5-15 mg) |
Spinal Anesthesia for Labor Pain
| Brand Name | Local anesthetic | Concentration | Dose (ml) | Opioid |
|---|---|---|---|---|
| Naropin | Ropivacaine | 5 mg/ml | 0,2-0,3 ml (1-1,25 mg) | Sufentanil 5 μg/ml 1-1,5 ml (7,5 mikrog) |
| Marcain Spinal | Bupivacaine | 5 mg/ml | 0,2-0,4 ml (1-2 mg) | Sufentanil 5 μg/ml 1-1,5 ml (7,5 mikrog) |

Addition of opioids in spinal anesthesia
| Local anesthetic | Concentration | Dose (weight units) | Dose in ml |
|---|---|---|---|
| Morpine | 0.4 mg/ml | 0,1–0,2 mg | 0,25–0,5 ml |
| Fentanyl | 50 mikorg/ml | 20–40 μg | 0,4–0,8 ml |
| Sufentanil | 5 μg/ml | 2,5–5–10 μg | 1–1,5 ml |
Obstetric Anesthesia Pocket Guide
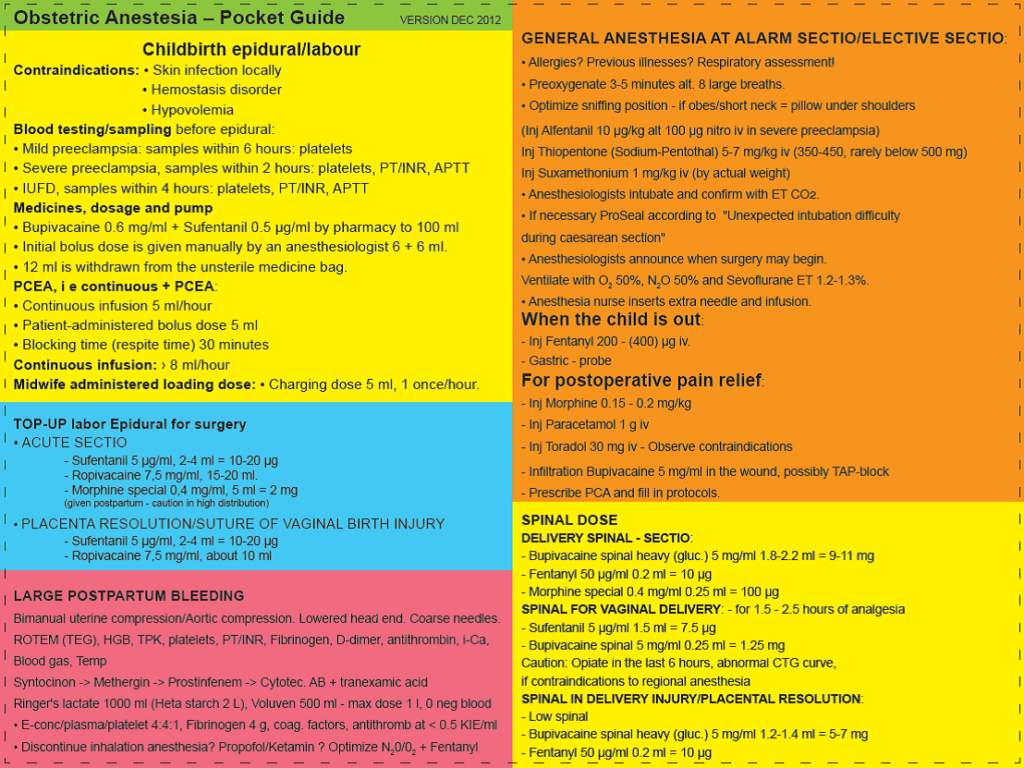
General Anesthesia for Emergency C-Section and Elective C-Section
Preliminary Preoperative Assessment:
- Allergies? Previous diseases? Quick airway assessment!
- Preoxygenate for 3-5 minutes or 8 deep breaths.
- Optimize sniffing position – if obese/short neck = pillow under the shoulder blades
Start of Anesthesia
- Propofol 2-2.5 mg/kg IV (200-250 mg)
- Thiopentone (Pentothal) 5-7 mg/kg IV (350-500 mg) or:
- Inject Suxamethonium (Succinylcholine/Celocurin) 1 mg/kg IV (based on actual weight) or
- Rocuronium in high dose
- (Alfentanil (Rapifen) 10 μg/kg or 100 μg nitroglycerin IV in severe preeclampsia)
- Anesthesiologist intubates and confirms with ET CO2
- If necessary, laryngeal mask (Pro-Seal) according to “Unexpected Intubation Difficulty during C-Section”
- Anesthesiologist informs that surgery can begin.
- Ventilate with O2 50%, N2O 50% and Sevoflurane ET 1.2-1.3%.
- Anesthesia nurse inserts an extra IV line and starts infusion.
When the baby is out:
- Inject Fentanyl 200-(400) μg IV.
- Nasogastric tube
- Syntocinon -> Methergin as per surgeon’s order
For Postoperative Pain Management:
- Morphine 0.15 – 0.2 mg/kg IV
- Paracetamol (Perfalgan) 1 g IV
- Ketoroloac (Toradol) 30 mg IV – Observe contraindications
- Infiltrate Marcaine 5 mg/ml into the wound, possibly TAP block
- Order PCA and fill out the protocol.
Obstetric Spinal Anesthesia
Spinal – C-section
- Bupivacaine Spinal Heavy (Marcaine) 5 mg/ml 1.8-2.2 ml = 9-11 mg
- Fentanyl 50 μg/ml 0.2 ml = 10 μg
- Special Morphine 0.4 mg/ml 0.25 ml = 100 μg
Spinal for Vaginal Delivery
The spinal provides approximately 1.5 – 2.5 hours of analgesia
- Sufenta 5 μg/ml 1.5 ml = 7.5 μg
- Marcain Spinal 5 mg/ml 0.25 ml = 1.25 mg
- CAUTION: Opioid in the last 6 h,
- Abnormal CTG curve, contraindication to regional anesthesia (?)
Spinal for Birth Injury / Placental Detachment:
– low spinal
- Marcain Spinal Heavy 5 mg/ml 1.2-1.4 ml = 5-7 mg
- Fentanyl 50 μg/ml 0.2 ml = 10 μg

Severe Postpartum Hemorrhage
Tests
- Rotem (TEG), Hgb, Platelet count (PLT), a-PTT, PT/INR, Fibrinogen, D-dimer, Antithrombin, Ionized Calcium, Blood Gas, Temperature
Actions
- Bimanual uterine compression/aortic compression
- Lowered head position
- Large-bore IV lines
- Syntocinon -> Methergin -> Prostinfenem -> Cytotec
- Antibiotics
- Tranexamic Acid (Cyklokapron) 2 g
Fluid Administration
- Ringer-acetate 1000 ml (caution >2 L), Voluven 500 ml – max dose 1 L
- O neg blood
- RBC/plasma/platelet concentrate in a 4:4:1 ratio
- Fibrinogen 4 g
- Antithrombin if <0.5 KIE/ml
- Possibly discontinue inhalation anesthesia
Anesthesia Type
- Propofol / Ketalar?
- Optimize N2O/O2 + Fentanyl
Thiopenthone (Pentocur/Pentothal)
Ultra-short-acting intravenous anesthetic that is a barbiturate derivative. Thiopenthone induces sleep when given intravenously. It induces hypnosis and anesthesia, but not analgesia. Primarily used for the induction of anesthesia for surgery but also for short medical procedures where short-term sleep is desired. It is usually administered as a manual injection with a syringe (25 mg/ml) where the speed and dose are adjusted according to the patient’s condition and the nature of the procedure. Thiopenthone can be given as a continuous infusion in the treatment of status epilepticus and elevated intracranial pressure due to cerebral edema. Thiopenthone was the standard agent for anesthesia induction for several decades but has recently been replaced by propofol and other anesthetics. It causes a dose-dependent depression of respiration and circulation. Thiopenthone is only a hypnotic and not a true analgesic, but pain relief is somewhat achieved with the depth of anesthesia. For surgical anesthesia, thiopenthone is usually supplemented with strong opioids such as fentanyl in balanced anesthesia. Compared to propofol, thiopenthone does not provide the same relaxation in the upper airways, which can lead to some rigidity and difficulties in manual ventilation. A small dose of thiopental can be given to prevent or treat laryngospasm.

Concentration: 25 mg/ml.
Pentothal is delivered and stored as a dry substance and is usually diluted to a fresh daily concentration of 25 mg/ml. The diluted solution has a shelf life of only 24 hours and should be stored in a refrigerator.
Dosage
Anesthesia induction: 4-6 mg/kg. The normal dose for a 70 kg patient is approximately 14 ml (± 4 ml) = 350 mg. A typical induction dose for adults is 4-6 mg/kg body weight, but individual responses vary so much that no fixed dosage can be specified. Typically, between 200 and 400 mg is given as an induction dose (8 – 16 ml at 25 mg/ml), with a default of 14 ml. In patients with poor general condition, the dose should usually be reduced and carefully titrated. After intravenous administration, unconsciousness occurs within 30 seconds and lasts for 20-30 minutes after a single dose. Rapid uptake occurs in most vascular areas of the brain, followed by redistribution to other tissues. It is rarely justified to give more than 500 mg intravenously. Thiopental has a distribution half-life of 2-4 hours after a single intravenous dose and an elimination half-life of 9-11 hours. Plasma protein binding is 80-90% at therapeutic concentrations.
Cave
Porphyria, upper airway obstruction, asthma attack, extravasal and intra-arterial injection. Pentothal causes histamine release, and a transient skin redness (usually over the chest and neck) can be seen after intravenous injection.
Caution
Caution in severe obesity, hypovolemia, hypotension, or severe shock.
Brand Names
Pentocur, Thiopental (discontinued).
Disclaimer:
The content on AnesthGuide.com is intended for use by medical professionals and is based on practices and guidelines within the Swedish healthcare context.
While all articles are reviewed by experienced professionals, the information provided may not be error-free or universally applicable.
Users are advised to always apply their professional judgment and consult relevant local guidelines.
By using this site, you agree to our Terms of Use.

