Author:
Kai Knudsen
Updated:
1 September, 2025
Electroencephalography (EEG) is a diagnostic method that records the electrical activity of the cerebral cortex via electrodes placed on the scalp. EEG is used in neurology, neurosurgery, and intensive care medicine to diagnose epilepsy, monitor consciousness, detect encephalopathy, and evaluate the effects of sedation and anesthesia. The method is non-invasive, has high temporal resolution, and is particularly useful for detecting dynamic changes in brain function.
Electroencephalography (EEG)
Indications
- Epilepsy: diagnosis, classification, follow-up
- Emergency and ICU: status epilepticus, refractory seizures, sedation/anesthesia monitoring
- Encephalopathies: metabolic, infectious, hypoxic-ischemic
- Disorders of consciousness: differentiation of coma, minimally conscious state, brain death
- Surgical monitoring: epilepsy surgery, neurosurgery, intraoperative monitoring
Technique and Methodology
- Electrode placement: standardized according to the 10–20 system, with electrodes positioned proportionally across the scalp.
- Recording: measures voltage differences between electrodes, amplified and displayed by the EEG machine.
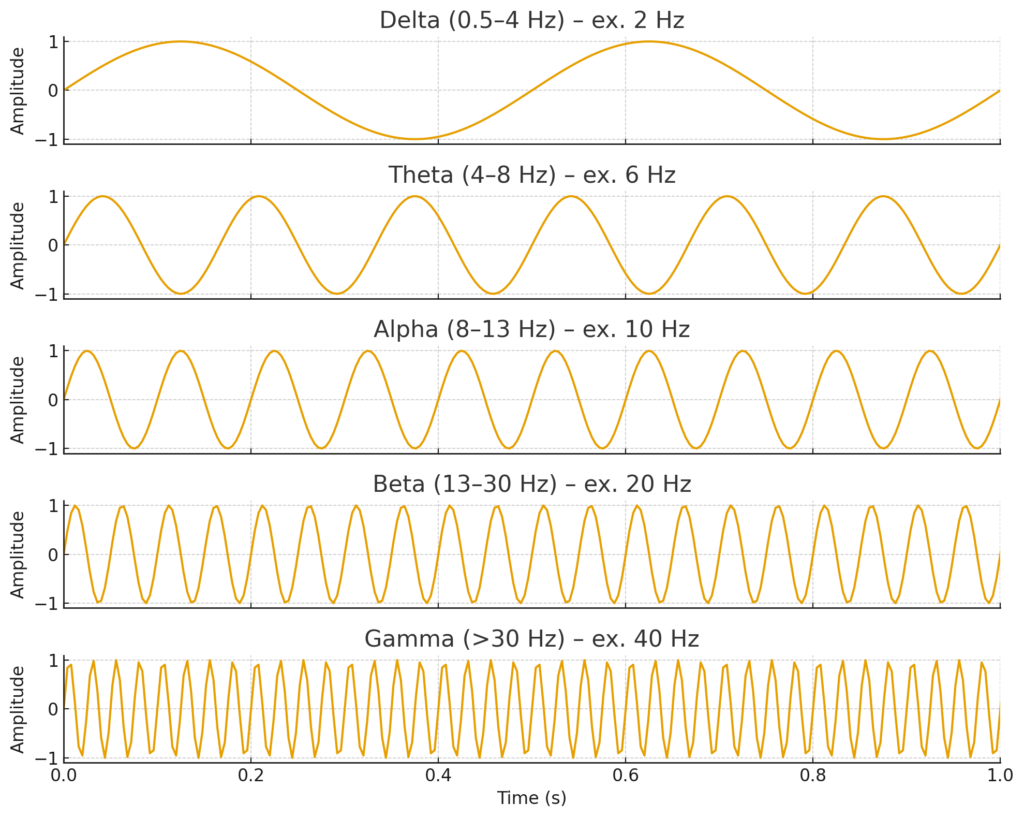
- Frequency bands:
- Delta (0.5–4 Hz): normal in infants and during sleep; pathological in adults (e.g., encephalopathy).
- Theta (4–8 Hz): normal in drowsiness; pathological in focal or diffuse cerebral dysfunction.
- Alpha (8–13 Hz): typical in relaxed wakefulness with eyes closed; attenuates with eye opening or mental activity.
- Beta (13–30 Hz): normal in wakefulness; increased by benzodiazepines and barbiturates.
- Gamma (>30 Hz): high-frequency oscillations with roles in cognition and epileptiform activity.

Interpretation
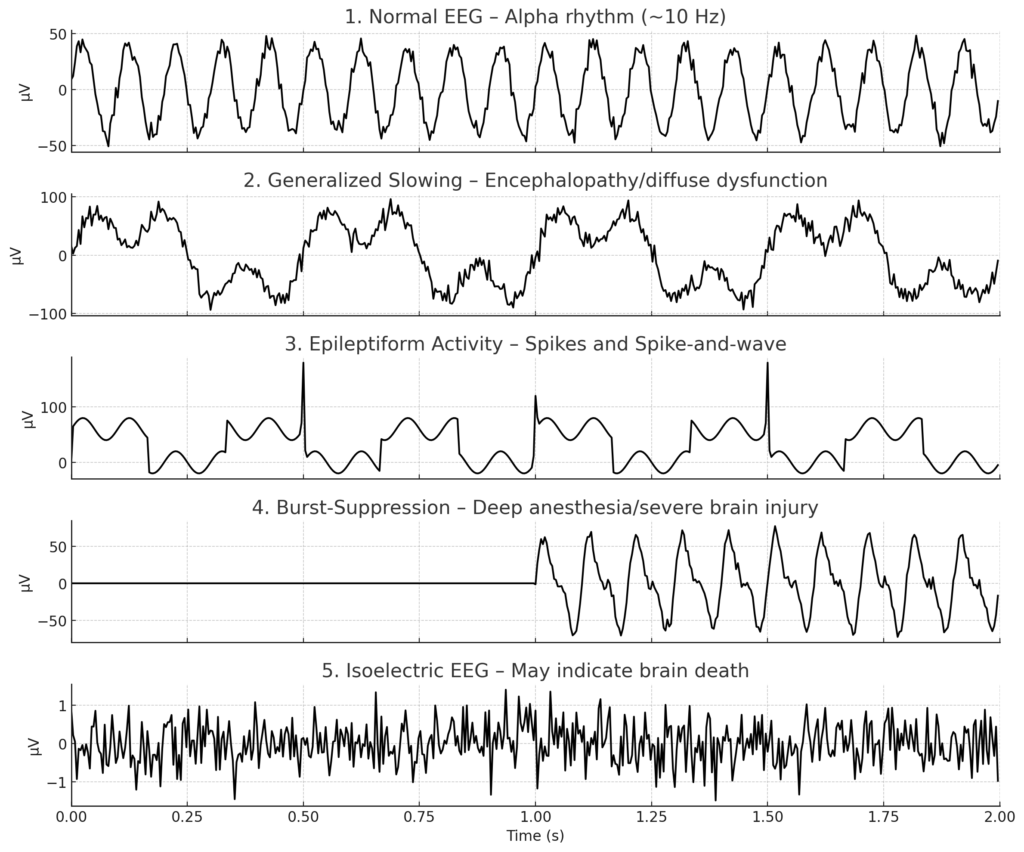
EEG interpretation must always be performed in relation to clinical context and history. Common findings include:
- Normal EEG: organized background rhythm with age-appropriate alpha activity.
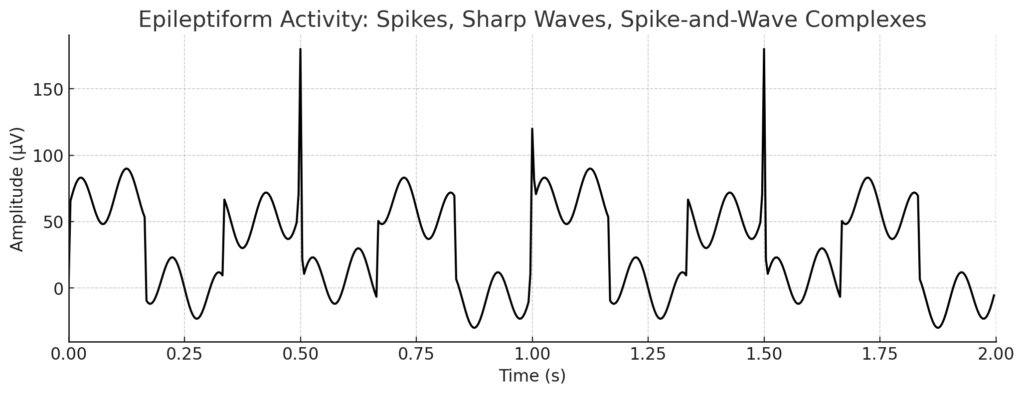
- Epileptiform activity: spikes, sharp waves, spike-and-wave complexes.
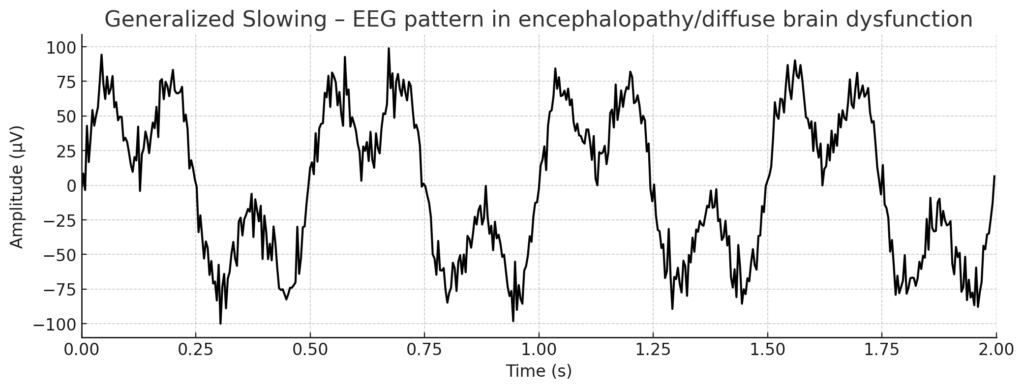
- Generalized slowing: sign of encephalopathy or diffuse brain dysfunction.
- Focal slowing: indicates localized lesion (e.g., tumor, stroke, scar tissue).
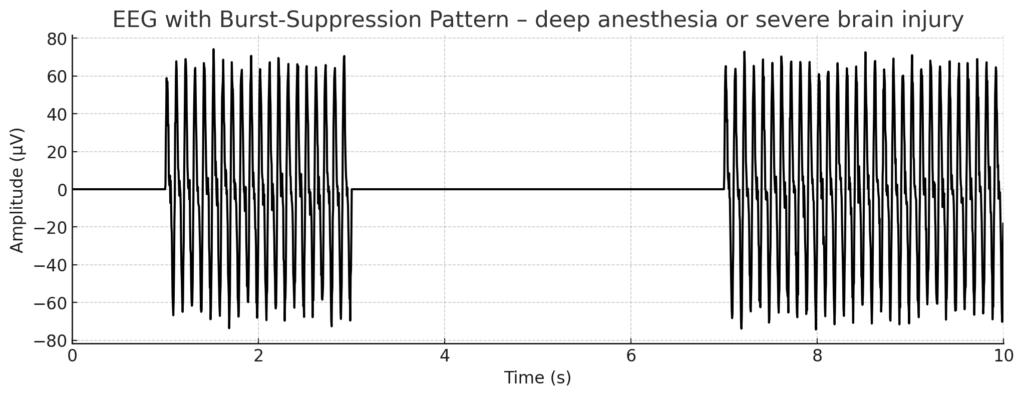
- Burst-suppression pattern: seen in deep anesthesia or severe brain injury.
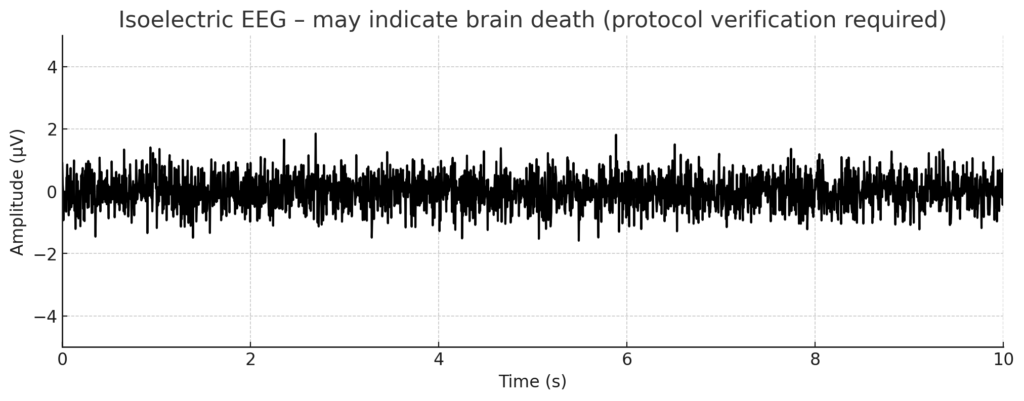
- Isoelectric EEG: may indicate brain death (requires protocol-based verification).

Specific Applications
Epilepsy
EEG is central in diagnosis and classification:
- Generalized epilepsy: bilateral spike-and-wave complexes.
- Focal epilepsy: localized spikes or rhythmic discharges.
EEG may be normal between seizures; prolonged or video-EEG monitoring is often required.
Intensive Care
- Continuous EEG monitoring (cEEG): used to detect non-convulsive status epilepticus, monitor sedation, and assess prognosis after cardiac arrest.
- Bispectral index (BIS) and other EEG-derived indices are used for anesthesia depth monitoring but differ methodologically from clinical EEG.
Encephalopathies
- Metabolic/toxic encephalopathy: diffuse slowing, triphasic waves.
- Hypoxic-ischemic encephalopathy: ranging from slowing to burst-suppression or isoelectric EEG depending on severity.
Limitations
- Lower spatial resolution compared with MRI/CT.
- Susceptible to artifacts (muscle activity, eye blinks, electrode noise).
- May be normal between seizures in epilepsy.
Summary
EEG is a central diagnostic method in neurology and intensive care medicine. It enables rapid, dynamic assessment of brain function, particularly in epilepsy, status epilepticus, encephalopathy, and altered consciousness. Interpretation requires expertise and must always be integrated with the clinical picture.
Disclaimer:
The content on AnesthGuide.com is intended for use by medical professionals and is based on practices and guidelines within the Swedish healthcare context.
While all articles are reviewed by experienced professionals, the information provided may not be error-free or universally applicable.
Users are advised to always apply their professional judgment and consult relevant local guidelines.
By using this site, you agree to our Terms of Use.

